This post contains affiliate links which means we earn a small commission if you purchase through these links.
Something I think many school nurses might struggle with is orthopedic assessment. Someone comes in crying with an injury but how do we know what we might be working with and what we should do about it?
The most common types of orthopedic injuries that we would see with kids at school are of course broken bones, sprains and strains, shin splints, ACL injuries, and traumatic brain injuries (TBI, concussions). Concussion is a conversation for another post but we will go over some basic possible fracture assessment for this post.
Despite what many people think, nurses do not gain x-ray vision in nursing school.
Common types of fractures
- Non-displaced: the bone is cracked but stays aligned.
- Stress: Small cracks in the bone usually from repeated stress such as running or gymnastics.
- Buckle: Not a true fracture but happens when the bone is compressed such as a fall on an outstretched hand and the bone bends and causes injury but does not break.
- Displaced angulated: Full break, bones are out of alignment and on an angle.
- Displaced translated: Full break, bones are out of alignment with each other but not angled.
- Displaced Rotated (spiral): Full break, bones moved in a twisting motion when breaking.
- Displaced greenstick: Partial break, one side breaks and the other side bends much like bending a fresh stick from a tree.
- Comminuted: Full break, bone is in multiple pieces.
- Compression: Like a buckle fracture, bone is compressed hard enough to collapse in on itself. This can happen from falling on outstretched hands, falling from a high height and landing on feet, or a car accident when the passenger’s feet are up on the dashboard.
- Open: Fracture that involves the bones breaking through the skin.
- Closed: Fracture that does not break the skin.
- Growth Plate Fracture: A break in the bone over the growth plate in children.
Common pediatric fractures:
(Links on each area to the Boston Children’s Hospital patient education forms) found here: https://www.childrenshospital.org/conditions/fractures
Shoulder, upper arm
- clavicle fracture: Fractured collarbone
- supracondylar humerus fracture: Fracture to the lower part of the humerus (upper arm bone) closer to the elbow.
- humeral shaft fracture: Fracture to the humerus (upper arm bone).
- proximal humeral fracture: Fracture to the upper part of the humerus (upper arm bone) closer to the shoulder.
Elbow
- occult elbow injury: A possible fracture to the elbow but is too difficult to see on x-ray.
- olecranon fracture: Fracture of the pointy part of the elbow, part of the ulna (one of the two forearm bones).
- medial epicondyle fracture: Fracture of the bottom of the humerus, in the elbow joint, on the inside part of the arm.
- lateral condyle fracture: Fracture of the bottom of the humerus, in the elbow joint, on the outside part of the arm.
Forearm
- bicoritical distal radial fracture: Full break of the radius (forearm) closer to the hand.
- distal radius buckle fracture: Buckle fracture of the radius closer to the hand.
- proximal radius fracture: Fracture of the radius closer to the elbow.
- distal radius growth plate fracture: Fracture of the radius through the growth plate closer to the hand.
- both-bone forearm fracture: Fractures of both the radius and ulna, the two bones of the forearm.
- radial shaft fracture and greenstick fracture: Fracture of the radius either full break or partially through the bone.
Hand, wrist
- metacarpal fracture: Fracture of the bone inside the hand that connects to the fingers.
- scaphoid fracture and occult scaphoid injury: Fracture of one of the bones that makes up the wrist.
Lower leg
- tibia fracture, toddler fracture, and Cozen’s fracture: Fracture of the tibia, one of the lower leg bones. Toddler fracture is a fracture in the middle of the tibial shaft usually in children under 3 years old, Cozen’s fracture is closer to the top near the knee.
- tibial shaft fracture and tibia-fibula fracture: Fracture of the tibia, Tib-fib is a fracture of both the lower leg bones.
- tibial tubercle fracture: Fracture of the tibia closer to the knee where the bone is more round.
Ankle, foot
- ankle fracture: Fracture of the lower part of the tibia or fibula closer to the foot.
- metatarsal fracture: fracture of the bones inside the foot that attach to the toes.
Symptoms of a possible fracture:
- Pain: pain can sometimes be referred to an area other than where the actual fracture is ie: hip fracture can present as pain to upper leg. Supracondylar humeral fracture can present as pain to elbow and forearm.
- Swelling: Edema to area surrounding injury.
- Obvious deformity: Sometimes fractures don’t always “look broken” but other times they look really broken. Obvious deformity requires x-ray.
- Difficulty moving limb or area in question: Range of motion may be decreased, inability to move limb or area in question without pain. In severe cases we won’t ask the patient to move the limb to assess but sometimes decreased ROM is obvious.
How to assess possible fractures
- Mechanism of injury including height of fall: What caused the injury? Did they fall from standing? Fall off a structure?
- Strength and Range of motion: Depending where the injury is located and how severe, assess if the person is able to move the area or not. Do they have pain when moving the area?
- Bruising
- Swelling
- Erythema
- Deformity: Is there an obvious area of deformity from the injury? Is the bone or limb bent at an abnormal angle?
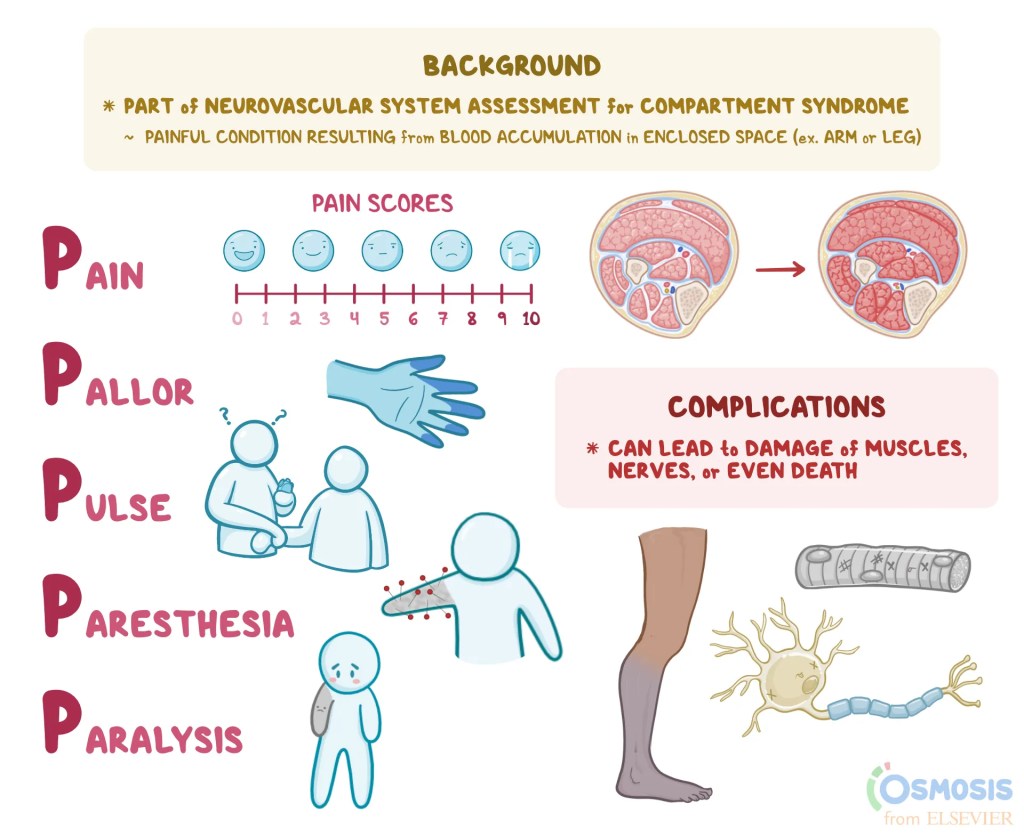
- Capillary refill: We are concerned about blood flow to the area if it is an arm or leg that is injured. Check capillary refill to assess for any compromise in blood flow.
- Distal pulses: Check pulses below the injury to assess compromise to blood flow.
- Distal sensation: Assess the level of sensation to the area below the injury. Can they feel your touch like normal? Not at all?
- Distal temperature: Assess the temperature of the limb below the injury. If it is cold or cool they may have a compromise in blood flow. Heat at the injury site can also be an indicator of a fracture.
- Pulseox: Check the pulseox if the injured limb is an arm. This is also to assess compromise of blood flow.
- Assess for other injuries: Check for other injuries such as head trauma, abrasions, bleeding, other possible fractures, or bruising, and address them as appropriate.
What to do with a possible fracture
- If fracture is suspected call the parents immediately. Call 911 depending on the severity of injury.
- Splinting: We aren’t splinting like they do in the ER but we do need to immobilize for comfort to get the student to to the ER for evaluation. This can be in the form of a pre-formed plastic splint and an elastic wrap, or even a cardboard splint and elastic wrap. The goal is stabilization and immobilization to prevent further injury. Alternatively, if injury is severe and splinting will cause more damage, do not move the person to splint, keep them comfortable and still until EMS arrives to take over.
- Ice: Ice will help reduce swelling and inflammation, can potentially decrease some discomfort as well.
In the Health Room
We have all been in a position where we have missed a fracture because it didn’t seem so serious when the student was in our office. Sometimes they don’t cry, they don’t have a ton of pain, they don’t have any obvious signs that would indicate a broken bone. I have learned the hard way to always report the injuries to parents even if it doesn’t seem serious. Give them a heads up that the student got hurt and while it seems ok right now the potential exists that it could change and require a medical evaluation. Write a note home, call them, send a text or a classdojo message, whatever it takes.
As I stated previously, we don’t receive our x-ray eyes in nursing school, we don’t know if something is broken or not without an x-ray.
Make sure you lay eyes on the injury even if it seems trivial. Take off the shoe, pull up the pant leg, take off the jacket and confirm the appearance of the injury.
Document the situation and assessment.
When is a possible fracture an emergency?
All possible fractures should be addressed emergently but some may require EMS attendance as opposed to waiting for a parent to transport to the ER.
- If the injury is caused by a major trauma like a fall from a structure
- If there is bone sticking through the skin.
- If the person is unable to move or you can’t move the injury without causing pain.
- If the injury involves the spine, neck, head or back.
- If the person is unresponsive
- If there is bleeding that can’t be controlled.
- If there are weak or absent pulses or neurovascular exam indicates compromise.
Check out these system assessment documentation forms on Teachers Pay teachers: https://www.teacherspayteachers.com/Product/School-nurse-health-assessment-forms-bundle-8525470
References:
- https://www.childrenshospital.org/conditions/fractures
- https://www.mayoclinic.org/first-aid/first-aid-fractures/basics/art-20056641#:~:text=If%20the%20broken%20bone%20is,there’s%20no%20breathing%20or%20heartbeat.
- https://www.osmosis.org/answers/distal-ulna-fracture
- https://www.saem.org/about-saem/academies-interest-groups-affiliates2/cdem/for-students/online-education/m3-curriculum/group-traumatic-and-orthopedic-injuries/orthopedic-injuries
- https://lms.rn.com/getpdf.php/2103.pdf


I think that this is a really great guide for new and seasoned school nurses. I would love to know more about your experience as a school nurse.
LikeLike