Remember when vaping and e-cigarettes came on the scene and everyone was thrilled that they could now “smoke” with virtually NO ill effects? So healthy! People indoors, “smoking” fruity flavored, cotton candy, apple pie flavored oils because it’s a healthy alternative to getting your nicotine in AND you can do it indoors right in people’s faces!
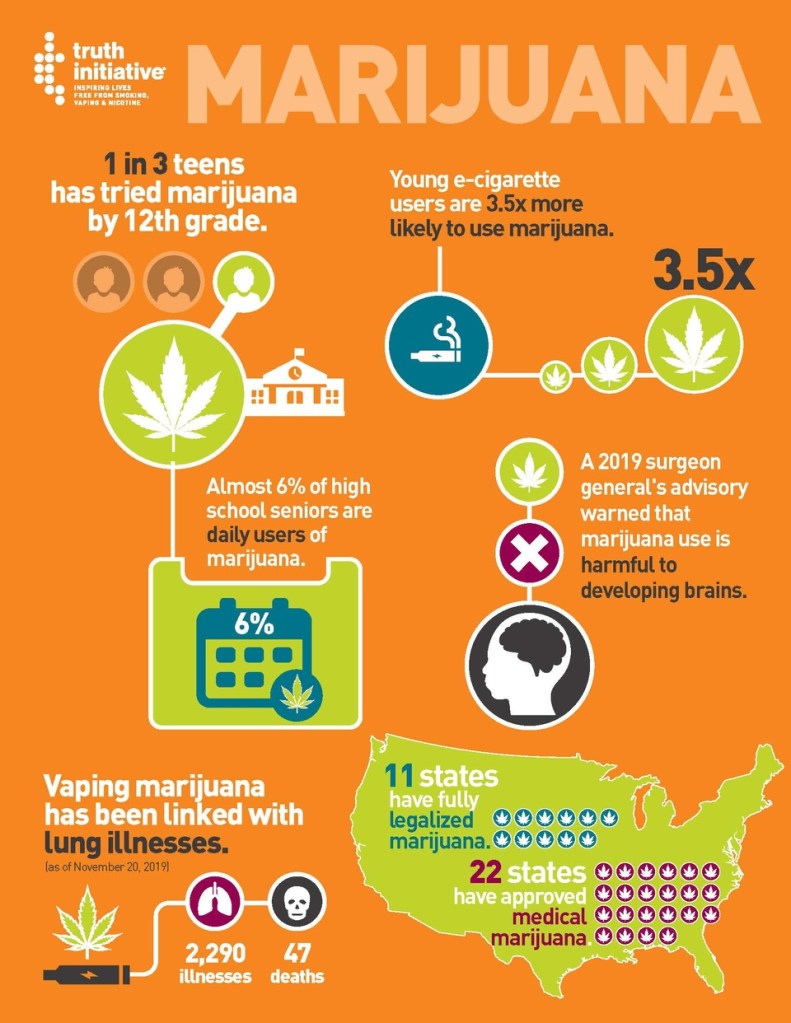
Later came new laws regarding marijuana legality in various states, dispensaries, and people vaping marijuana. It seemed like a great idea at the time for sure as there can be many benefits to using THC for various ailments from cancer pain, nausea from chemo, relaxing Parkinson’s tremors, relaxing tourette’s tics, managing severe autism, stimulating eating in a person with dementia, other pain like migraines and arthritis, to anxiety and PTSD.
So let’s get into it: the good and the bad of vaping. Yes, there is some “good” but in reality, after all the research that is being done, all the physical injuries related to vaping nicotine or THC the bad outweighs the good and it’s just not worth it.
Pros:
People started vaping oils and e-cigarettes as a way to cut down on the many many chemicals found in cigarettes. Smoking cigarettes expose you to literally thousands of dangerous cancer causing chemicals, puts you at risk for many forms of cancer aside from just lung cancer, and puts you at risk for heart disease, lung disease like COPD, stroke, and diabetes just to name a few.
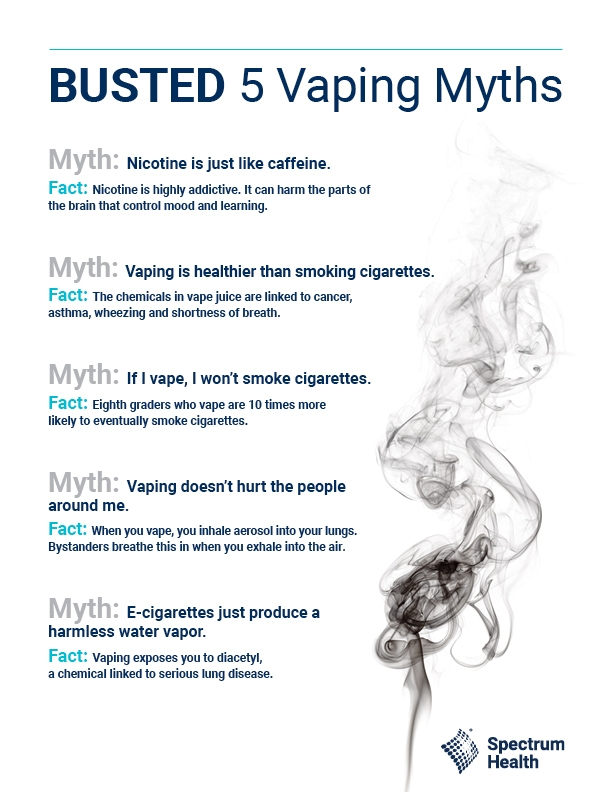
- Vaping exposes you to fewer chemicals than smoking cigarettes. This is also a con because vaping still exposes you to other different dangerous chemicals.
- Vaping does not expose you to tar or carbon monoxide like cigarettes do.
- If you’re vaping THC you get a better product delivery than smoking dry flower because it is more concentrated THC. This is also a con because a person who is new to using THC is more likely to have greater effects from vaping and is more likely to have greater side effects.
- That’s all the pros I’m gonna give because the reality is that there are no pros to vaping or smoking.
Cons:
- Vaping exposes you to different dangerous chemicals than smoking including Diacetyl, Formaldehyde, and Acrolein. These chemicals when ingested in the vaping oil can lead to severe lung damage and even death. In addition, the vape pens themselves often offer exposure to other dangerous chemicals and metallic compounds from the heating coils that can cause irreversible lung damage such as something called Bronchiolitis Obliterans aka Popcorn Lung.
- Many vape products contain propylene glycol and glycerin, which, alongside many other polycyclic hydrocarbons, are linked to the development of cancers and lung and cardiovascular diseases.
- Vaping with cartridges that are not from either a regulated dispensary or made in one’s own home have the potential to have other additives like vitamin E oil which can lead to permanent lung damage. Vitamin E is often used as a thickening and delivery agent in e-liquid. And, while it’s safe when taken orally as a supplement or used on the skin, it’s likely an irritant when inhaled. It’s been found in the lungs of people with severe, vaping-related damage.
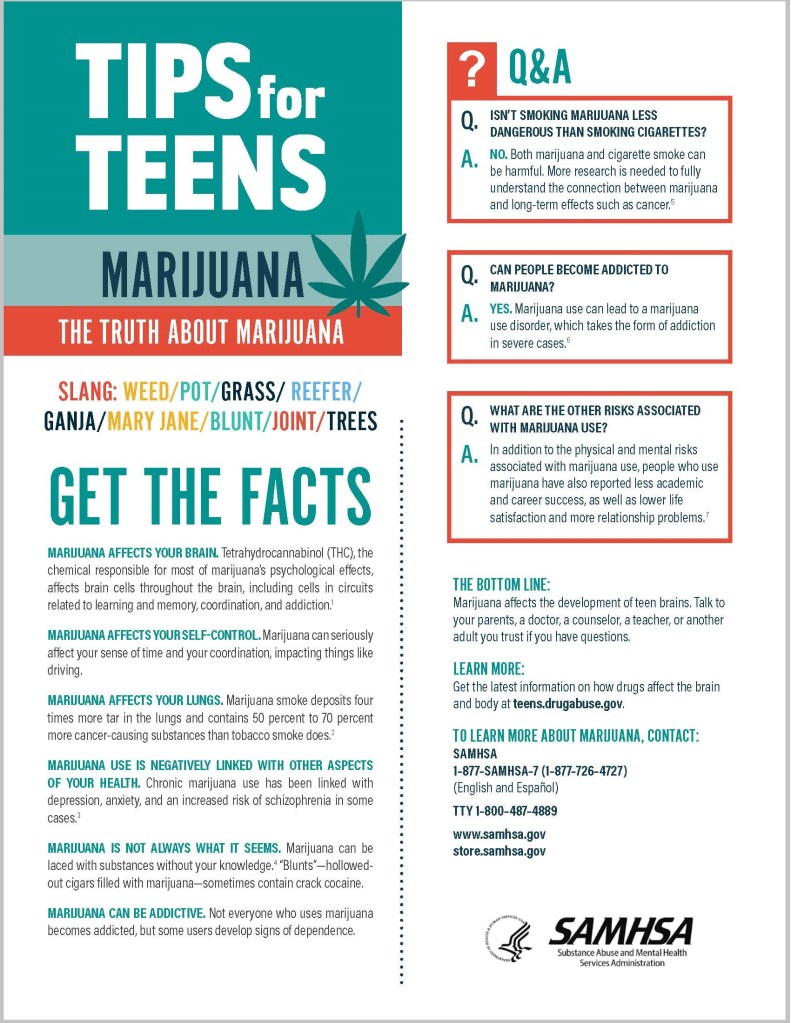
- Teens’ brains are not fully developed yet. Teens who are exposed to chemicals such as THC, Nicotine, Alcohol or other illicit substances are highly susceptible to cognitive deficits like memory problems, poor coordination, poor reflexes, poor decision making skills.
- Because of the lack of full brain development, teens are more likely to develop marijuana use disorder or addiction to marijuana. They are also more likely to develop poorer academic success, poorer career success, lower life satisfaction and increased relationship problems.
- Marijuana use as a teen can lead to increased depression, anxiety and increased risk for developing schizophrenia.
- It is a myth that the second hand “smoke” from vapes does not affect those around you. The people that you are vaping in front of are now breathing in the same harmful chemicals that you are breathing in and putting them at risk. So all those people who think it’s ok to vape indoors in front of people are putting everyone else at risk as well as themselves.
- Research has proven that switching to vaping does not in fact help anyone quit smoking.
What is in the vape juice/oil?
E-liquid, also called e-juice or vape juice, is what vaping devices use to make the vapor you breathe in. E-liquids aren’t just water. They usually contain:
- Flavoring. Each flavoring has its own set of ingredients.
- Nicotine, the addictive and harmful substance in cigarettes and other tobacco products.
- Propylene glycol and glycerin, used to create vapor.
E-liquids and flavorings sometimes have other ingredients, including:
- Chemicals that can cause cancer (carcinogens), like acetaldehyde and formaldehyde.
- Chemicals known to cause lung disease, such as acrolein, diacetyl and diethylene glycol.
- THC (tetrahydrocannabinol), the chemical in marijuana that gets you “high.”
- Vitamin E acetate, linked to lung injury caused by vaping (EVALI, see below).
- Heavy metals like nickel, tin, lead and cadmium.
- Tiny (ultrafine) particles that can get deep into your lungs.
Health problems associated with vaping
- Popcorn lung: Diacetyl, a chemical used in some flavorings, can cause bronchiolitis obliterans (“popcorn lung”). Bronchiolitis obliterans causes permanent scarring in your lungs. Popcorn lung gets it’s name from it’s discovery in people who worked in a popcorn factory who were breathing in Diacetyl and developed this permanent lung scarring.
- EVALI (e-cigarette, or vaping, product use associated lung injury). EVALI is a serious lung condition that vaping causes. It causes widespread damage to your lungs and gives you symptoms like coughing, shortness of breath and chest pain. EVALI can be fatal.
- Cancers: lung cancer, bowel cancer, many many forms of cancer can be caused by smoking or vaping.
- COPD: Asthma, emphysema, chronic lung disease. This is permanent.
- Heart attack/stroke: The increase in adrenaline and the decrease in oxygen flow can lead to heart attacks and strokes. You can literally die from this.
- Addiction: Many people think that marijuana is not addictive but it most certainly can lead to marijuana use disorder. Also nicotine is highly addictive.
- Injury from vape devices exploding or burning: Yep, that’s right, the devices can explode! They can also malfunction and burn you.
Alternatives:
- Quit. If you are vaping nicotine then quit. I know that’s not as easy and it sounds but there is no physical need for nicotine in any form. For help to quit smoking you can look here: https://www.lung.org/quit-smoking/i-want-to-quit
- If you are vaping THC or smoking flower for medical reasons, there are other methods of delivery for it than vaping or smoking such as edible, RSO, tinctures, creams and others. If you are using THC for recreation, it is legal for recreation where you live and you are of an appropriate age to use THC safely then again, there are other methods of delivery aside from vaping or smoking.
Additional facts about vaping
- The smell from THC vapes is extremely short lived. Be aware that teens can more easily take a few hits from a THC oil vape and go undetected than if they smoked whole flower.
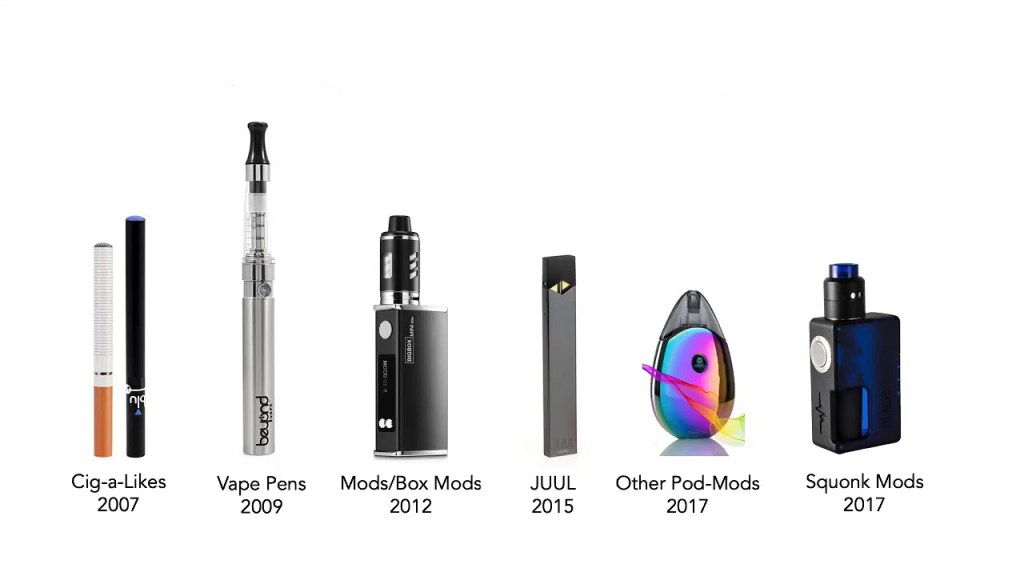
- The devices for vaping have developed into things that look like other things. They might look like a USB drive, a cell phone case, an actual pen, or even a smart watch. Some of the paraphernalia might be disguised as other items also such as lip balm (dabs are stored in little jars that could be mistaken for other things).
- 60% of young people think that vapes are mostly just flavoring while the reality is that 98% of them have nicotine.
- Researchers disagree on the statement that marijuana is a “gateway drug” as we were always taught in the 80’s and 90’s. There is little evidence suggesting that people who use marijuana continue on to using harder drugs although it is not impossible to imagine. That being said, marijuana use in teens is dangerous in itself anyway.
- Even if you have a high quality THC product, the vape devices themselves can cause chemical exposure from the internal workings of the heat coils and chemicals used to heat them up.
- It’s really expensive. Average cost to vape a JUUL – $1,008 PER YEAR; Average cost to vape refillable e-cigarettes – $1,512 PER YEAR. The average yearly cost of healthcare for e-cigarette users is $1.3 BILLION. Average cost of vape cartridges at a dispensary: $30-$50 and up!
Conclusion
It’s just not worth it. Vaping anything as a teen can seriously mess up your body and brain and affect the rest of your life. Vaping anything as an adult can seriously mess up your body and brain and also affect your life. For help and information about substance abuse visit https://www.samhsa.gov/.
Please like and follow my blog and comment with your thoughts on this topic!

References
https://leafwell.com/blog/are-all-cannabis-oil-cartridges-safe-when-vaped/
https://www.healthline.com/health-news/teens-and-disguised-vaping-devices