What is Commotio Cordis and Why Should a School Nurse Be Worried?
I’m sure everyone has heard of the devastating event with Damar Hamlin at the Buffalo Bills vs Bengals game last night. Damar took what appeared to be a not super hard shoulder to the chest during a play as probably happens a million times during a million football games but this time one was way more serious because he went into cardiac arrest almost immediately, collapsing on the field.
Because there are obviously trainers and medical personnel present, they identified cardiac arrest and began CPR almost immediately, also utilizing the AED and shocking him on the field. They were able to get a heart rhythm back and get him to the hospital for further treatment but he is presently in the ICU. The world is praying for a good outcome for this young, healthy athlete.
So what happened? The speculation regarding this event is that he suffered from something called Commotio Cordis (comm-OH-shee-oh COR-diss) which is a cardiac arrest after a blow to the left chest at the exact second the heart is entering the T-wave portion of the electrical impulse. The reasoning for assuming this diagnosis is that he took the shoulder to the chest and then almost immediately dropped on the field. He is a healthy, young man with no existing conditions, cardiac or otherwise, that would give concern for a cardiac event.
I will preface the further information by stating that I am NOT a cardiac nurse by any means so when I heard this was the probable diagnosis I had to start researching. I remember learning about this in nursing school and during my emergency trauma training but I didn’t remember the specifics. I remembered learning about this when I was a medical assistant in pediatrics and one of the doctors experienced a similar event while working as a medical consultant for a Little League baseball game when a young player took a pitch to the chest while not wearing a chest pad.
So what is Commotio Cordis? In a nutshell, a person receives blunt force trauma to the left chest during the exact moment that the T-wave is beginning causing an interruption in the cardiac repolarization of the ventricle thus scrambling the electrical impulse causing depolarization instead and causing the heart to go into ventricular fibrillation (v-fib) which is a non sustainable cardiac rhythm.
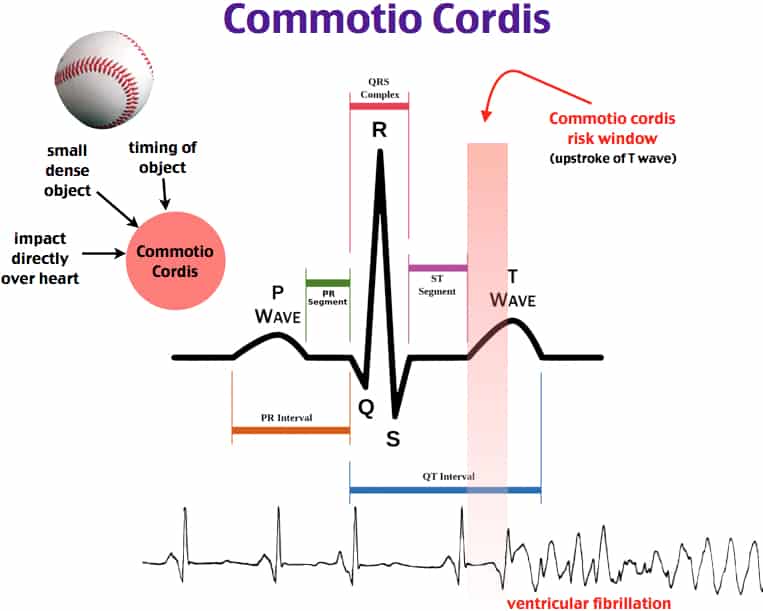
As we’ve all learned from nursing school and BLS/ACLS training, v-fib leads to cardiac arrest and v-fib is a shockable rhythm. This is why it is so incredibly important to have a working AED available, especially during any sports, PE class, or even recess where kids are playing and running around. It is equally as important for people (including students) to have BLS training because the sooner you start perfusion the better the outcome will be after cardiac arrest.
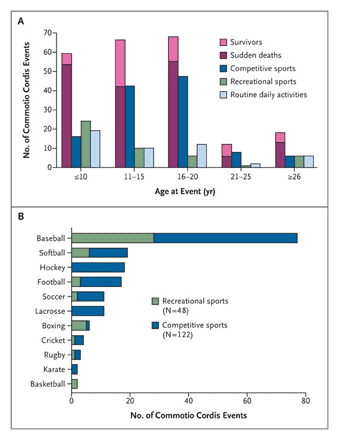
Commotio Cordis (CC) is most commonly associated with baseball/softball players as they run the risk of being hit directly in the chest with a fast moving ball. Additionally it is associated with hockey puck, lacrosse ball, soccer balls, cricket balls, and hockey sticks as they all have the likelihood of a fast moving direct hit to the chest. Also, any blow to the chest from a tackle, a punch (boxing, MMA fighting, martial arts), or even car accident can also cause CC.
Commotio Cordis treatment includes:
- Rapid recognition of cardiac arrest
- Immediately beginning CPR/chest compressions
- Call EMS
- Retrieve AED and defibrillate as soon as possible.
Can it be prevented? Yes, if proper safety precautions are taken then it can be prevented or treated quickly. Following these steps will help:
- Have an athletic trainer present at practices and games
- Educate coaches, parents, and athletes how to perform CPR and use an AED
- Educate coaches, parents, and athletes of signs of commotio cordis
- Have an AED accessible near playing fields at all times
- Ensure coaches know where to locate the AED
- Ensure there is an Emergency Action Plan in place
- Ensure protective equipment is properly fitted
- Teach athletes how to avoid being hit with a ball/puck
- Avoid strength disparities among participants and coaches
- Use safety baseballs
So why should a school nurse be worried about this? While it is fairly rare (less than 30 cases reported per year) it is always a possibility during any kind of physical activity that could cause trauma to the chest. Along with sports trainers and coaches, PE teachers, and anyone supervising physical activities and sports, we should be ensuring that people have CPR training and there are working AEDs accessible in the building. It is important that students are also educated in sudden cardiac arrest, CPR, and AED usage as there have been cases where it was the young student that saved another student or staff member’s life because of their fast thinking and knowledge of CPR.
As the school nurse be sure to consider what is the person wearing? Football pads? Baseball pads? How will you get through those to begin CPR? My suggestion for the fastest way is either trauma shears (keep them with the AED) or begin CPR with the pads on (make sure you’re giving GOOD compressions) and then cut off the clothes when the AED arrives.
Make sure there is a plan in place in the case of sudden cardiac arrest and that those present know their role and how to access the needed equipment and help. Ensure that AEDs are marked clearly and that everyone knows where they are, make sure there is someone who knows how to do CPR present. Every second counts, the longer everyone is debating what to do the longer the patient is without perfusion. Immediate CPR gives the better outcomes.
Here are some visual explanations of Commotio Cordis:
https://ksi.uconn.edu/emergency-conditions/cardiac-conditions/commotio-cordis/
https://www.ahajournals.org/doi/full/10.1161/circep.111.962712
What do you want to see more of?
I wrote a book!! Head to Amazon to check it out! https://amzn.to/3WHSYke
Tummyaches: When should I be concerned?
Tummyaches. Maybe one of our most common complaints and one of our biggest enigmas. Is every kid with a tummyache or an episode of throwing up sick? Short answer: no. Long answer: it depends on a lot of factors. Let’s discuss.
Stomachaches can come from a number of issues (this is not an exhaustive list):
- Appendicitis
- Stomach virus
- Menstrual cramps
- Stress or anxiety
- Hunger
- Indigestion/reflux
- Known diagnoses such as Crohn’s, Ulcerative Colitis, irritable bowel disease, feeding problems, or reflux to name a few.
- Constipation
- Urinary tract infection
- Strep throat
- Food allergies, sensitivities and intolerances
- Medications
- Pregnancy
When presented with a student complaining of a stomachache or vomiting we need to ask a few questions:
- Where does it hurt exactly? Point with one finger to the spot. This helps us know if we need to delve in further to determine if they need to be evaluated for appendicitis (lower right quadrant), if they have to poop (upper and/or lower left quadrants), or if they are hungry/have indigestion possibly (periumbilical/epigastric), if it’s menstrual (pelvic/cramps), or even if it’s just some anxiety (generalized all over “hurts”). Obviously we can’t diagnose any of these things specifically but we can pinpoint any areas of concern and decide what we need to do to help them.
- What were they doing when the stomachache started? Were they running around at recess right after eating lunch and got a stitch in their side or upset stomach? Were they doing something in class that caused them to worry a little too much (like a test or a difficult subject)? Was it right after having pizza or Takis or something that would cause some indigestion? Or were they happily going about their day when it struck them?
- If the complaint includes vomiting: what preceded the vomiting incident? Did they choke on food? do they have a bad cough that made them throw up? Did they witness someone else throw up and throw up also in solidarity? Did they see or smell something gross that made them throw up?
- Did they throw up a little bit or a lot? We all know they will always say they threw up a lot. What I want to know is was it just a little bit in your mouth? All your food on the floor? A little bit of mucus that you spit out? Unwitnessed trashcan and bathroom throw ups are often more like spit-ups that are misconstrued as “vomiting” to the younger kids.
- How do they feel now? Still nauseated? Gonna throw up again? Stomach still hurts? Or are they all better now that it’s over?
- Does it hurt when they go pee? Kids might have pelvic pain or belly pain related to a UTI which would possibly cause dysuria in addition to the belly pain.
For further assessment we want to consider:
- Do they have a fever?
- Do they have accompanying diarrhea?
- When is the last time they went poop? Little ones mostly do not remember when that was but worth asking.
- Do they have an existing health issues that might contribute such as food allergies, UC, IBS, Crohn’s, lactose intolerance, or taking meds?
- Watch them walk or ask them to jump in place and watch their face: do they have increased pain with jumping or walking type movement? This would be indicative of potential appendicitis.
- If everyone is comfortable with it you can have the student lie down and you can palpate the belly and see if they have any pain on palpation. Note where the pain is if any.
- What was for lunch and breakfast today? What was for dinner last night? Have they been eating? Do they have access to nutritious food?
- Do they have other symptoms such as sore throat and/or headache or rash? Signs of strep throat can include stomachache, headache, sore throat, vomiting, sandy textured rash to trunk, and fever.
- Observe how they look right now. Are they pale or greenish? Do they look sick? Is their demeanor normal?
- If it is appropriate to ask, it would be helpful to know if the student uses marijuana or any other illicit drugs. Chronic use of marijuana has been known to lead to cyclic vomiting syndrome or Cannabinoid Hyperemesis Syndrome which includes severe abdominal pain and uncontrollable vomiting. Use of some other drugs and withdrawal from them can also lead to intractable abdominal pain and vomiting as well. Role of chronic cannabis use: Cyclic vomiting syndrome vs cannabinoid hyperemesis syndrome
- If applicable and appropriate to ask, is the student pregnant or possibly pregnant?
- Are there any concerns of eating disorders in the student?
Now that you’ve asked a zillion questions and checked them out, what can you do about their complaint of tummyache?

- Send them to the bathroom to try and poop. In my experience most kids don’t want to poop at school which I completely understand but always worth a try. If pooping is a continuing issue for the student then you can recommend that the parent try a probiotic to help their digestive system. I love Garden of Life vitamins.
- If allowed in your district try Tums antacid if it seems like indigestion. An alternative would be sucking on a peppermint. My caveats with peppermints are to be aware of the risks: consider the ingredients in the candy and students religious beliefs and dietary limitations (Halal, kosher, food allergies and intolerances etc), be aware that peppermints pose a risk for choking.
- Health counselling: educate students on choosing healthy foods or non-spicy foods if they are having possible indigestion related to diet. If they are having limited access to food then that should be addressed as soon as possible.
- Allow them to take a rest for a bit. Give the student 10 minutes to lie down and rest and often they will feel better and be ready to go about their day.
- Give a snack if appropriate. If the student hasn’t eaten today for whatever reason try giving a snack such as crackers (presuming they are not allergic or personally averse to the ingredients), or ginger ale (again presuming that is appropriate for the specific student).
- Give PO fluids. Drinking a little bit (or a lot) or water can help often.
- Give hot/warm tea if permitted. Chamomile tea, or non caffeinated ginger tea can help calm the stomach.
- If permitted for your school/district try ginger candies. Ginger is an excellent stomach calmer and many pregnant people swear by it for nausea. Keep in mind that again, candy poses a risk for choking, allergies, and could potentially be against religious beliefs depending on the ingredients. I personally would consult the parent prior to giving this and have not actually given ginger candies at school but it is always an option to explore. Here is an article about ginger and nausea.
- Try having a “yucky bucket”. Take a gallon jug, clean it well, cut off the top and you have a barf bucket with a handle! You could potentially have one per classroom if you can collect enough of them. Sometimes just having the attention of the bucket and seeing the nurse does the trick. You can also use dollar store buckets but recycling old milk jugs is nice for the environment too.
- Obviously if they give concern for a more serious issue like appendicitis you would be calling their grown-ups immediately for evaluation. You would be calling EMS if indicated.
- If they are actively sick and vomiting then call their grown-ups and home they go!
- If suspicious for any other issues then manage accordingly, ie: pregnancy, UTI, strep throat. Call grown-up and recommend visiting the doctor. Follow your state laws regarding pregnancy and drug related issues and privacy. Here is an article from AAP discussing minors and privacy laws for your reference.
- When in doubt always call the parent and run it by them to see what they think. Sometimes having the student speak to the parent helps the student get themselves together to get back to class also.
- Avoid giving meds like Ibuprofen or Aleve because they will make abdominal pain and/or vomiting worse. If they have a fever and you need to give meds then stick with Tylenol if it is appropriate and allowed for that student.
- Try using a heating pad or a hot water bottle on the belly. Sometimes the heat can relax the muscles and relieve cramping related to menstruation, or vomiting and diarrhea.
- Here is a great article about home remedies for stomachaches with explanations: https://www.parentcircle.com/effective-home-remedies-for-stomach-ache-in-children/article

Do you have any advice, tips, or tricks for bellyaches that I didn’t mention? Follow and message me and let me know!
https://www.aafp.org/pubs/afp/issues/2008/0401/p971.html#
https://schoolnursing101.com/acute/abdominal/
https://www.wikihow.com/Get-Rid-of-a-Stomach-Ache-at-School
https://www.parentcircle.com/effective-home-remedies-for-stomach-ache-in-children/article
All About Pinkeye
Pinkeye: how do we know when we need to react to real pinkeye and when we can leave it alone because it isn’t actually pinkeye? What even is “pinkeye”?
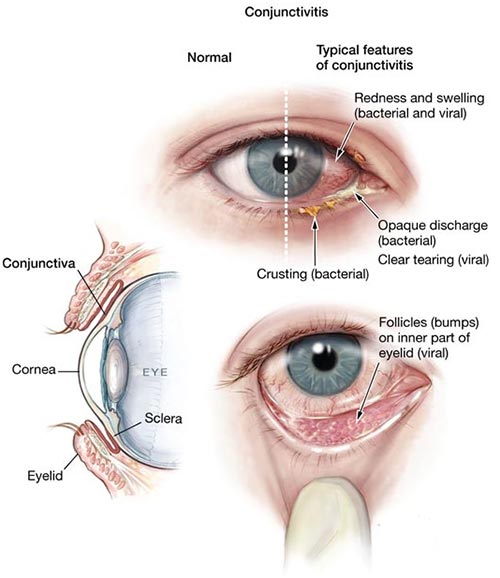
Warning: there is a gross picture of an eye coming up for the ommetaphobics out there.
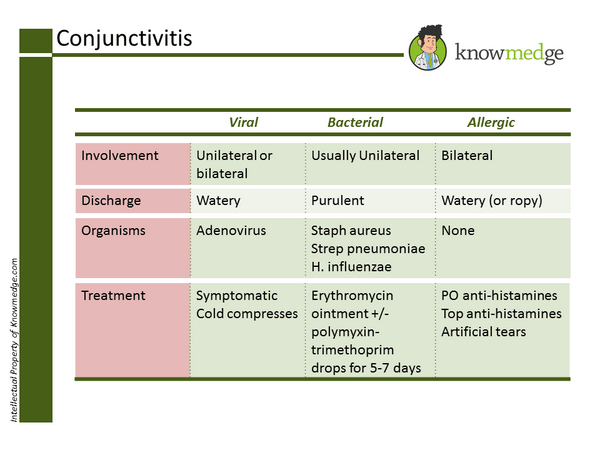
To start, “pinkeye” is a blanket term used to describe all forms of conjunctivitis: an inflammation or infection of the conjunctiva – the clear membrane that covers the eye and and also the inside of the upper and lower eyelids. It can be a viral infection, bacterial infection or allergic. Viral and bacterial conjunctivitis are very easily spread by physical contact with the drainage from the person’s eye while allergic conjunctivitis is not. Conjunctivitis can also be caused by an irritant such as chemicals, foreign bodies in eye or in infants by a blocked tear duct.
Some main symptoms of pinkeye are:
- Redness of the whites of the eye (the sclera)
- Itching of the eye
- Thick sticky mucusy drainage that tends to “glue the eye shut” in the mornings – more than just the normal eye boogies we all get
- A “gritty” feeling in the eye like there is dust in it,
- There can be swelling of the eyelids or even the sclera
- Increased redness and swelling of the inner lower eyelid if the eyelids are pulled down gently as pictured below.

So you have a student standing in front of you with a complaint of “red eye”. What can you do with this? We can not diagnose the type of conjunctivitis of course but we should know when to send them to the doctor and when we can send them back to class.
- How does the eye feel? is it itchy? painful? gritty? normal?
- Did they have lots of goop this morning? Do they have lots of goop now?
- Did they get anything in their eye just now like eraser dust, regular dust, dirt/sand, chemicals (soap, sanitizer etc), pool chlorine, cigarette smoke or other environmental pollutants?
- Do they have other cold symptoms like a runny/stuffy nose, coughing, or increased allergies?
- Do they wear contact lenses and do they take proper care of them?
- Have they just had an injury to the eye such as getting poked or hit in it?
- With a gloved hand you can gently pull down the lower eyelids and compare if the red one is also swollen and red inside the lower eyelid compared to the normal eye or if both eyes are affected they could both be excessively red and/or swollen.
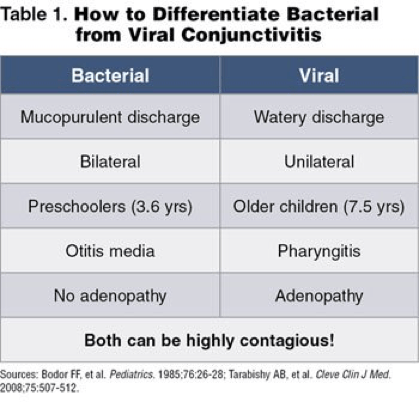
If you’ve determined that it is probable infectious pinkeye based on the questions and exam then the student should be sent home to be seen by a doctor for official diagnosis and treatment (if applicable). For my district and many others the student must be treated for 24 hours before they can return to school if they are diagnosed with bacterial conjunctivitis. For viral and allergic they may return to school immediately if desired.
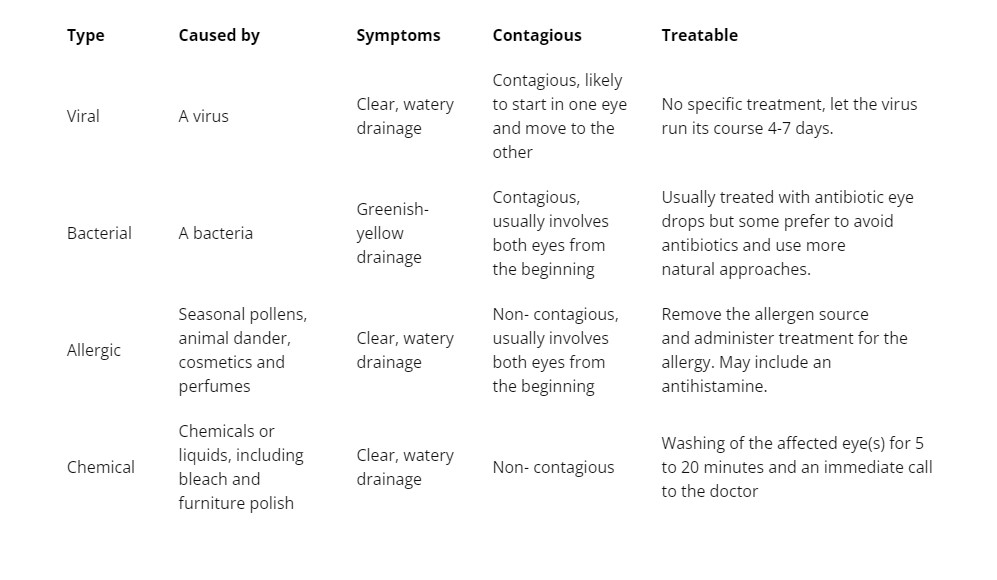
Treatments for bacterial conjunctivitis may include:
- Antibiotic drops or ointment such as Erythromycin, Ciprofloxacin, or Tobramycin
- Discontinue use of contact lenses until treatment course is finished, use new lenses after treatment is finished.
- Artificial tears eye drops
- Steroid eye drops such as Tobradex (combo Tobramycin and Dexamethasone) or Prednisolone drops.
- Warm compresses to remove the excessive drainage.
- Ibuprofen can help with pain and inflammation
- If available a parent may choose to use fresh breastmilk on a cotton ball as a compress to treat bacterial conjunctivitis, especially in infants less than 6 months old. Obviously this is not a treatment to be used at school but at home if the parent chooses to. https://pubmed.ncbi.nlm.nih.gov/33098117/
- Bacterial pinkeye often is accompanied by a strep throat or otitis media infection. If a child has one they may also develop the others as well.
- Prevent it from spreading to others by avoiding touching your eyes, washing hands frequently, not sharing eye drops or makeup with others.
- Change pillow cases and face towels often and throw out any mascara or eyeliner that may be contaminated in order to prevent reinfection.
Treatment for viral conjunctivitis may include:
- There is no specific medication to treat a viral infection.
- Steroid drops if the symptoms are severe
- Warm compress for comfort
- Artificial tears for comfort
- Antiviral medication if the doctor determines that the infection is related to Herpes Simplex virus.
- Discontinue contact lenses and use a new pair once infection is cleared up.
- Ibuprofen can help with pain and inflammation
- Allow the symptoms to run its course.
- Viral pinkeye usually accompanies a cold.
- Prevent it from spreading to others by avoiding touching your eyes and washing hands frequently.
Treatment for allergic conjunctivitis:
- Allergy medications such as Zyrtec, Allegra, Claritin etc.
- Allergy eye drops such as Pataday or Systane
- Avoiding exposure to the possible allergen if possible.
Treatment for other non-infectious conjunctivitis (chemical or foreign body exposure):
- Remove contact lenses if applicable
- Flush eye well for several minutes with water. You can use an eye wash found here or here.
- call poison control if unsure about the chemical exposure https://www.poison.org/articles/help-for-poisons-splashed-in-the-eye
- Seek emergency care as per poison control recommendation or if symptoms are severe. Certain chemical exposure to the eyes can cause scarring, damage to the eye, and possible loss of sight or eye if not properly addressed.
For all types of conjunctivitis it is wise to avoid using any oils, herbs, folk remedies etc (except for the breastmilk – that one is scientifically proven!) as most of these are not sterile or researched or doctor approved and could potentially cause permanent damage to the eye.
At the end of the day, we nurses cannot diagnose or treat conjunctivitis on our own and need a physician’s input. We should be aware of when a student needs to be referred for treatment and what types of treatments we should expect the student to have after they’ve seen the doctor.
Check my TPT for letters to send home informing parents of pinkeye exposure and other great resources!
https://www.cdc.gov/conjunctivitis/clinical.html
https://kidshealth.org/en/parents/conjunctivitis.html?ref=search
https://www.mayoclinic.org/diseases-conditions/pink-eye/diagnosis-treatment/drc-20376360
https://www.aao.org/eye-health/diseases/pink-eye-conjunctivitis
https://the-eyedoctor.com/blog/2021/9/8/6-things-you-never-knew-about-pink-eye-mysteries-revealed
https://www.healthline.com/health/how-to-get-rid-of-pink-eye-fast
An Open Letter to the Powers That Be… Send Help!
School nurses are facing burnout like never before. In the aftermath of the Covid pandemic where healthcare workers went from mildly respected to “heroes” and now villains enforcing the rules, the school nurses have been overwhelmed and beaten down with heaps of expectations and very little help.
In addition to our regular jobs of managing students’ diverse health needs and chronic conditions, immunization compliance, day to day injuries and illness, helping students with their mental health, helping teachers with their mental health, clerical work that is expected to be done, and organizing screenings we have been also tasked with Covid testing (schools with 400 – 2000 students), contact tracing, quarantine enforcement, mask enforcement, organizing classroom quarantines and masking, keeping up with the ever changing rules and protocols for managing Covid in schools and being the knowledge ambassador of all things Covid.
Many of us spent almost a year working from home trying to navigate how to be a school nurse from home while some of us spent that year continuing to work in our school buildings directly facing the deadliest time of Covid with little to no support or even recognition. We then went into a full school year loaded with new and changing Covid protocols, nonstop positive cases that required coordinating the logistics of contact tracing and quarantining hundreds of students and teachers sometimes.
No one noticed.
The immense pressure put on us to not only be the person with all the knowledge because we are the Registered Nurses but to singlehandedly coordinate the mitigation efforts in our schools has caused many of us to have greatly increased anxiety (22%), depression (24%), PTSD (30%), and felt bullied and harrassed related to our jobs (48%!!!). Many school nurses have quit or decided to retire. It is a dire situation when school nurses would rather retire early or go to work in the hospital where they feel they will be more respected and treated better (those that have experience working in the hospitals know how bad it has to be to make that choice.)
We need help. We can not do this alone! We need to ensure that there is a nurse in every building, and for some more than one nurse. We need extra nurses and subs to help cover absences (because nurses get sick too and have families that get sick). We need competitive pay to ensure the newer school nurses will stay and to make it worthwhile for us to stay. We need to be evaluated and supervised by school nurse leaders who understand our position. We need a professional ladder of career growth specific to school nurses. We need assistance paying for the education we are required to have specific to school health. We are human, we need understanding and patience and respect.
For those admins and parents who have supported us, we thank you from the bottom of our hearts. This hasn’t been easy for anyone but we are all doing the best we can with what we’ve got. We need the continuing support and understanding of the school and district admins and the parents. For those that feel like it is ok to threaten, harass, refuse to comply please understand that we are doing our best to follow the protocols that we are given by the Health Department and the CDC. We aren’t making the rules but it is our job to ensure that they are followed to the best of our abilities.
The results of this survey filled out by school nurses are scary to say the least.

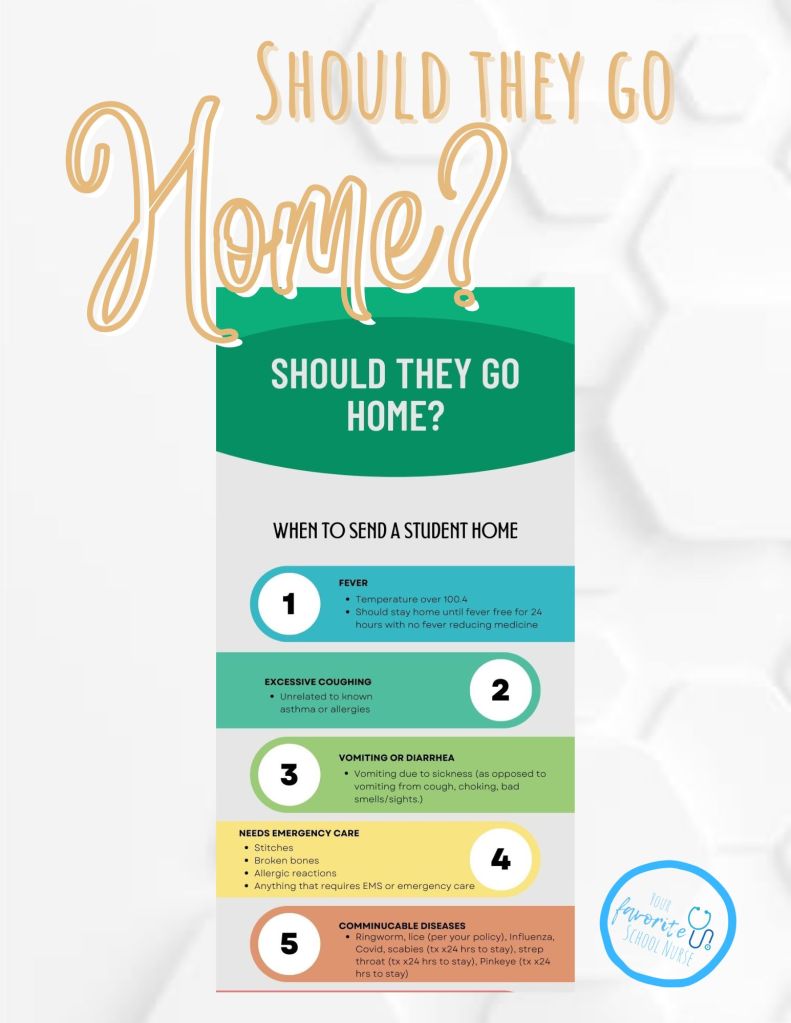
When Should You Send a Student Home?
A question I’ve seen asked by a few CSN’s recently is “How do I know when a student should be sent home versus sent back to class?” Is there a specific formula to make that decision? The short answer is no. Every situation is individual and every kid has different needs so what might send one kid home might not send another kid home.
Before I get into specific guidelines to consider, I want to point out two things: 1. Listen to your teachers. They are with these students most of the day and they know when they are not themselves. Often the students trust the teachers and confide in them if something needs addressing. Don’t just assume that the teachers are “trying to do your job” because most of the time they are just trying to do theirs. It’s a team effort. And 2. You’re the boss of your health room. Don’t feel pressured into sending students home or keeping them at school. You do your assessment, you make the medical decisions.
Sending a student home should be considered when the health issue is impacting their ability to learn in class.
So here are some basic guidelines that can be used to decide if they should stay or if they should go. This is not an exhaustive list as it is dependent on the student at the time.
Fever: If the student has a fever over 100.4 they should go home (in some places the rule is still 100.0 because of Covid). In most schools they should not return until they are fever free for 24 hours with no fever reducing medications. They should not be given fever reducing medications and sent to school, or be given medication and sent back to class. Also consider Covid testing.
Excessive coughing: cough unrelated to known asthma or allergies that is disruptive and causes inability to focus on class. If they are coughing up a lung and miserable then send them home. Check a temp and consider Covid testing.
Vomiting or diarrhea: If a student is vomiting due to sickness they should go home. Often you will find little ones that saw something gross that made them throw up, or they gagged on their food and have a low threshold for vomiting – in cases like that they can get themselves together and return to class. Consider how they look (pale, clammy, feverish, in pain, etc), how they report that they feel (tummy hurts? Gonna throw up again?). Check a temp and consider Covid testing. If the student is having diarrhea they should be sent home.
Needs emergency care: Injuries that require sutures should be picked up as soon as possible and have that addressed immediately. Broken bones or suspected broken bones should be picked up as soon as possible for emergency evaluation. Anything that requires the activation of EMS for the problem obviously should not be in school ie: anaphylaxis, use of Epinephrine, asthma attack that is difficult to control,
communicable disease (diagnosed or suspected): Obviously we can’t diagnose but there are a few things that we can send home for suspected concern such as suspected pinkeye, suspected scabies, suspected strep throat, lice – per your district policy as many districts are not excluding immediately for lice, and obviously Covid if they are tested at school and test positive.
Pinkeye: while we can’t diagnose pinkeye we can assess for the obvious signs for it such as eye redness, swelling, copious discharge, intense itching, and pull down the lower eyelid to look for increased redness or swelling inside the lower eyelid. Pinkeye can be viral or bacterial but we won’t know until they see a doctor. Due to it’s highly contagious nature, the student should be sent home to be evaluated.
Seizure: While not all seizures require the student to be sent home, some can. In general, absence seizures are fairly benign and the student can continue their day. Some grand mal seizures can cause the student to urinate or defecate on themselves, or require emergency medications or EMS calls in which cases they should obviously be sent home. Some students who have a seizure may be postictal but be allowed to remain at school. That is an individual issue that should be addressed with the parent and student as part of their action plan.
Asthma: most of the time a student with an asthma flare can be treated and return to class. On occasion the measures at school are not enough to treat the flare and the student may need to be picked up to be closely monitored by their guardian and possibly seek medical care or use their nebulizer at home.
Diabetic Emergencies: high and low blood sugars can generally be treated at school and the student can return to class when stable but if they are having a difficult day with managing or they are very out of control and symptomatic then the parent can be called to pick them up to closely monitor at home and/or seek medical care (or EMS if appropriate)
Certain head injuries: obviously minor head bumps do not need to be sent home but a more severe head injury with other symptoms such as change in consciousness, needs sutures, severe pain, or dizziness would need to either be sent home with parent for medical evaluation or sent to hospital.
Sickle Cell crisis: Often sickle cell issues can be managed at school with a little bit of rest, hydration and Tylenol but if the symptoms are more severe or not settling with the usual measures then the student should be sent home. If a Sickle Cell student develops a fever the parent should be notified immediately as per their action plan.
Covid: Districts all have varying rules regarding Covid protocols but in general if a student tests negative at school but is symptomatic then they should be sent home to see the doctor and have a PCR test or an alternative diagnosis.
CSN’s clinical judgement: The CSN is here to make these decisions. If the nurse examines the student and feels that they are sick and need to be sent home then there you have it. Sometimes the nurse (and teacher) knows that the student is not a complainer or that they don’t look right or seem like themselves.
Again, this is not an exhaustive list of when to send a student home. Most of the time it’s a judgement call but your safest bet is to call the parent and let them decide what they want to do if you are unsure if they should stay or go. Districts all have varying guidelines as to certain protocols like lice and covid so look into the specific protocol for your district or state to be sure.
Would you add anything to this list? Message me and let me know what you think!
First Aid for Nosebleeds for the School Nurse
This post contains affiliate links which means we earn a small commission if you purchase through these links
One of our most favorite things: the bloodbath that ensues when a student gets a random nosebleed at school and runs through the halls to the nurse for help, all the while leaving a trail of blood in their wake. What’s a busy school nurse to do?
First thing’s first: we need to get that under control then we can ask questions about what happened and what they were doing when it started. Did they get punched in the face? Is it super hot inside or outside? Do they have allergies? Were they picking? Is it winter and the forced air heat is on drying everyone’s mucus membranes out? Did they stick something up there? Do they maybe just get nosebleeds sometimes when they are stressed or upset? Very importantly, do they have a bleeding disorder (hemophilia, Von Willebrand’s)?
Back to getting the bleeding under control: Here are some conventional and unconventional tips.
- Grab some tissues or paper towels (preferably NOT those waterproof brown ones we all know so well) and get to pinching the lower part of the nose so the nostrils are closed. Instruct the student to tip their head FORWARD not backward. Leaning forward will reduce pressure on those veins allowing them to form clots and lighten the bleeding some. Additionally, leaning forward will help avoid getting the blood in their throat potentially causing choking, aspiration, and upset stomach.
- Continue to pinch the nose for a good 5-10 minutes. You can try using a clothespin or a nose clamp to help pinch the nose correctly, or just pinch with a gloved hand.
- If there is a large clot in the nostril you may have the student gently blow and remove that and then continue pinching the nose until bleeding stops.
- Try putting ice on the bridge of the nose. Putting ice in this spot will help constrict the blood vessels and slow or stop the bleeding.
- Try putting ice on the back of the neck. While the scientific research does not support this, it is said that ice on the back of the neck can constrict the blood vessels in the nasal mucosa. It might not work but many feel that it does and it can’t hurt right? People also swear by using cold keys or a cold butter knife on the back of the neck in a pinch. https://www.baltimoresun.com/news/bs-xpm-2008-05-01-0805010077-story.html
- Try putting ice in the mouth – ice cubes or popsicles. Have the student try to hold the ice on the roof of their mouth with their tongue. According to physician responders to an article in the British Medical Journal, ice packs to the neck or nasal bridge are less effective than placing ice in the mouth. https://www.bmj.com/content/344/bmj.e1097/rapid-responses
- Try the “thumping the foot” method. You determine which nostril is bleeding, then remove the shoe from the OPPOSITE foot and give two whacks with the heel of your hand to the heel of the bare foot (not so hard that you hurt them though!). Alternatively, have the child stomp their foot on the ground hard with the opposite foot from the bleeding nostril. Again, this is a non-scientific method but allegedly it works!
- Try placing a cotton roll or rolled up gauze under the top lip inside the mouth and give a little pressure to the upper lip frenulum.
- Try wetting a teabag and placing it on the outside of the nose or inside the nostril. Black tea contains a natural antiviral called Quercetin and also the tannins in black tea can help reduce bleeding and inflammation. You may have also heard of using this method after teeth have been removed to help with bleeding and pain. https://www.home-remedies-for-you.com/askquestion/45354/remedy-for-nose-bleeds-with-tea-bag.html
- Try comercial nosebleed products that should stop the bleeding (if you are allowed to use them in your health room) like nasal gels, quickseal nose plugs, or the Bleedcease brown seaweed things. Use at your own risk though, these types of products may not be approved for use in the school health room but might be helpful at sports or at home.
- Try the old wives tale of placing a copper penny on the forehead while also pinching the nose and tilting forward. No one knows why this allegedly works but people swear by it. Maybe it is related to the cold near the blood vessels helping them to constrict or maybe it’s just buying time for the bleeding to stop on it’s own. There is no scientific merit to this but perhaps we will experiment and see…
- Do not use nasal sprays at school for nosebleeds. This may be the standard of care in an ER or at home but it is not appropriate to use medications at school. That being said, at home an adult can try using Afrin nasal spray or a nasal spray with Phenylephrine to constrict the blood vessels and stop the bleeding. Again, this method is not for use at school by the school nurse for kids.
- You should try to avoid using packing, tampons, or things that are inserted into the nose to stop a nosebleed. This will have to be removed later and can cause more bleeding when removed. Leave the nasal packing to the ER docs. https://www.med.umich.edu/pdf/Nosebleed-Dos-and-Donts.pdf
Now that the bleeding has stopped, What should we do going forward?
- Once the bleeding is under control, the nurse can carefully put some plain vaseline into the nostril to moisturize the mucus membrane using a long cotton tipped applicator. This will not always stop the bleeding but can prevent further damage from dry nasal passages causing increased bleeding. Neosporin also works but for many it is considered a medication and thus prohibited for use in the health room without an order.
- If it is permitted in your district you can give some nasal saline in the nose to help moisturize.
- Instruct the student to refrain from picking their nose, sticking tissues or anything up there, and not to blow their nose for a while after to prevent re-bleeding.
- Inform the parent about the nosebleed and instruct them to use vaseline, saline nasal spray, and if possible a cool mist humidifier at home if it is a dry air season.
When is a nosebleed an emergency?
- When the bleeding does not stop by 30 minutes.
- When the bleeding is so heavy that it is pouring down the throat and out of the nose causing a potential choking hazard.
- When the patient is lightheaded, pale, or has a decreased level of consciousness.
- When the nosebleed is accompanied by severely elevated blood pressure, rapid heart rate, chest pain or lightheadedness.
- When the patient is on blood thinners.
- When the patient has a bleeding or clotting disorder such as hemophilia or Von Willebrand’s.
- When the nosebleed is caused by a severe head or facial trauma.
https://kidshealth.org/en/parents/nose-bleed.html
Do You Use a Wood’s Lamp in Your Health Room?
I want to preface this post with the caveat that as registered nurses we are not able to diagnose any condition but we can perform our examination and give recommendations as to what we believe the issue might be. The students would always have to follow up with a doctor or nurse practitioner for diagnosis and treatment.

A Wood’s Lamp is an ultraviolet light or “blacklight” that comes in many sizes and shapes and can be used to check for certain skin conditions, head lice, or corneal abrasion (which we would not be doing at school as that is a procedure to be performed by a doctor). The Wood’s lamp was invented in 1903 by physicist Robert Wood. It was used starting in 1925 to diagnose fungal infections in the hair and has found practical use ever since. It is frequently used by estheticians and dermatologists to examine skin and skin conditions.
What would we use the Wood’s lamp for in the health room?
Head lice/nits: live nits (lice eggs) will glow white under the woods lamp. empty nit cases will glow grayish. This can help determine if the student is suffering from dry skin or hair product flakes (will not glow under the lamp), or if the white spots in the hair are nits. Live lice can be seen without the light but will also glow.

Ringworm and Tinea Capitis (ringworm on the scalp), Pityriasis Versicolor or Tinea Versicolor (fungal skin infection) and other fungal skin infections: While it seems fairly obvious what ringworm looks like through the naked eye (red circle, clear in the center, maybe flaky), the Wood’s lamp can help confirm that the student needs to cover the area and see a doctor as soon as possible. This fungal infection on the skin would glow bright blue-white or yellow-green under the lamp. While it might be beneficial to know ringworm vs other fungal infections, again, we can’t diagnose so a generic “likely fungal, need doctor to evaluate and treat” is sufficient. No need for specific diagnoses.

Scabies: Will fluoresce under woods lamp. No diagnosis can be made but strong suspicion can be suggested and recommend seeing doctor for evaluation and treatment.
Bruises: Bruises don’t glow but you can see the demarcation of the bruise and often get a better idea of the shape and size under the lamp if needed. Honestly, I would be unlikely to be examining a bruise that closely in a school health room setting. If anything, I would be using this knowledge to determine something like if it is a bruise or if it is a stain on the skin.
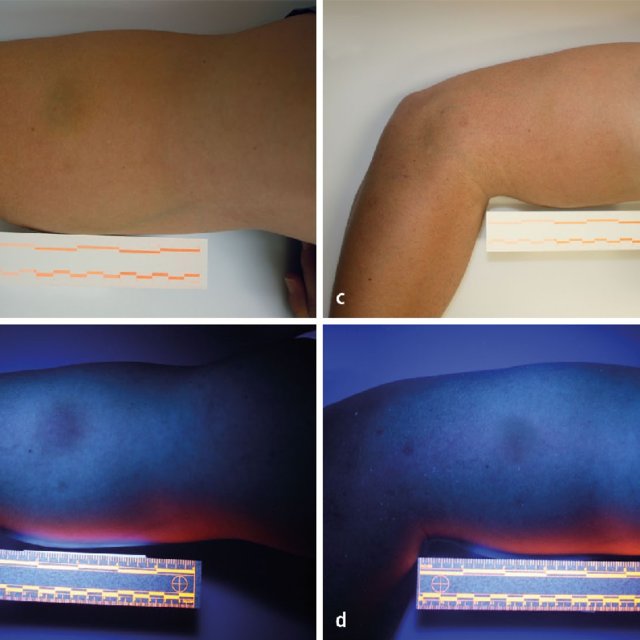
Urine: Glows yellow/green under the blacklight. Again, I would be unlikely to be determining urine stains vs other fluid stains in a school health room setting but the need for this knowledge could come up for some reason.

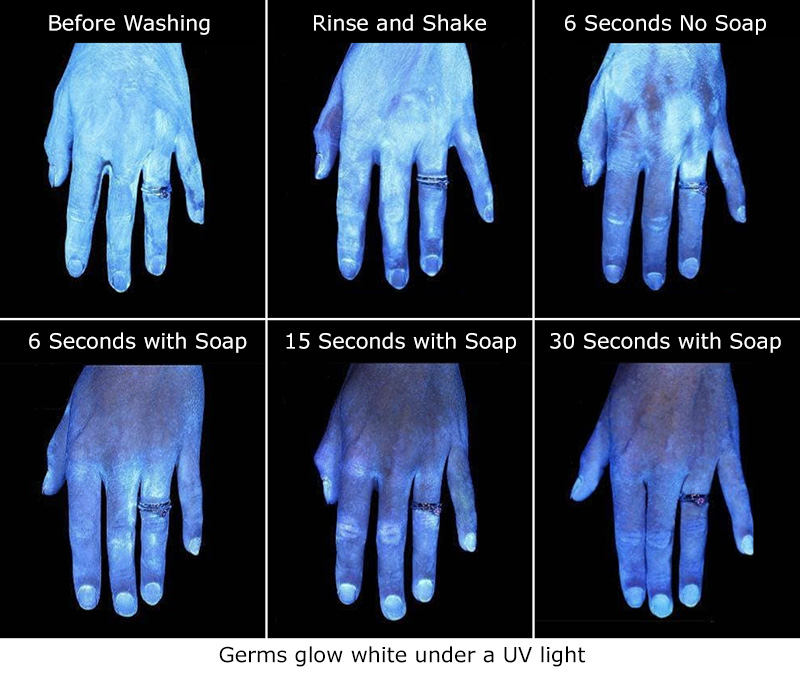
Germs: a blacklight or a Wood’s lamp can show poorly or unwashed hands! A great educational tool for students to show the importance of washing hands and how germs are spread.
A Wood’s Lamp can also show a corneal abrasion with the use of Fluorescence strips, however, a school nurse can not perform that examination and would require a doctor, PA, or NP to perform, diagnose, and treat.
Procedure:
- Have the client position themselves comfortably.
- Explain to the client that the Wood’s light has the same characteristics as a typical black light; the room will be darkened, and the black light will be turned on to examine for fluorescence of the lesion in question.
- Have all lights turned off.
- Ideally with a real Wood’s Lamp (as opposed to a blacklight) the lamp should warm up for approximately 1 minute before using to have the best visualization.
- Hold the Wood’s light approximately 6 to 8 inches from the lesion in question, and observe the characteristics of the fluorescence of the lesion.
Where can you get your own Wood’s Lamp?
I got a little rechargeable one from Amazon found here (click the picture to link to the product):
Amazon also has many options or battery powered, corded, or rechargeable lithium ion battery. (Click the pictures for links to the products):
If you buy your supplies for SchoolHealth.com you can try some of these options also:
TL/DR
- Woods Lamp can look for conditions such as ringworm, other fungal skin infections, lice, scabies, bruises, urine, and clean hands, among other concerns.
- School nurses can not diagnose any conditions but this is a helpful tool for us to point a parent in the right direction if needed.
Sources:
https://www.healthline.com/health/woods-lamp-examination
https://www.verywellhealth.com/what-is-woods-lamp-examination-5212402
https://www.usamedicalsurgical.com/blog/top-9-medical-diagnostic-applications-woods-lamp/
http://www.djj.state.ga.us/Policies/DJJPolicies/Chapter11/Attachments/DJJ11.30AttachmentF.pdf
https://www.statpearls.com/ArticleLibrary/viewarticle/31386
file:///C:/Users/Teacher/Downloads/Superficial_Fungal_Infections.pdf
https://thenurseszone.com/woods-light-examination/