Calling all the stressed out school nurses trying to navigate through the real emergencies, paperwork, screenings 504’s and IEP’s and minor injuries/illnesses! Are you inundated with kids who sneezed once or bumped themselves on a desk or door? Kids with loose teeth or dirty clothes?
We school nurses have a ton to deal with all day. It can definitely get difficult to get through it all. An important helpful factor in managing your health room is communication with teachers and staff. Everyone needs to be on the same page.
Teachers and other staff have the right and the ability to triage students they are sending out of their classrooms and make a determination as to whether it is an emergency or can wait. They are allowed to tell the student with a stomachache to wait, or tell the student with a loose tooth to wait it out and stay in class. The goal is to keep the kids in class anyway right?
You need staff to understand and respect your health room hours and allow you to wade through all the work you have for each day. One way for them to help you is to understand what things are actually an emergency and what isn’t. It’s understandable that someone who isn’t medical may not know how to handle possible medical issues but at the same time, they are teachers and they know the kids and can make that determination in most cases.
The first thing you need to do is to establish set health room hours and let everyone know. It can be tough to get everyone to follow the hours if you haven’t already established something like this. I have made multiple signs which I email out to the staff periodically and also have posted in multiple areas in my school – including my door. Your health room hours can be whatever works for you. If you need to give yourself two hours in the morning to get your screenings and computer work done and an hour or so in the afternoon to get documentation done then do what works. Some people are more comfortable having an open door policy or a locked door policy.
Next, you have to establish what is considered an emergency and what is not. Understandably, many people who are not medically trained have no idea what is or isn’t an emergency and may think that everything or nothing is an emergency. You can communicate this information to all staff to help be sure everyone is on the same page.
Some examples of emergent reasons to be seen by the school nurse are:
1. Bleeding: excessive bleeding, difficult to control bleeding, needs more than just a band-aid. Paper cuts, small scrapes, etc can either wait until the nurse is available or a staff member can dispense a band-aid if one is available.
2. Breathing Bad: Short of breath at rest, asthma, wheezing. “Out of breath” from playing at recess or gym or sports is not an emergency.
3. Broken: Obvious broken bone, excessive swelling, inability to walk or use body part. Banged knees, bumped elbows, other minor bumps and hurts can wait.
4. Barfing: Vomited more than once, witnessed by staff, visibly ill. A kid who reports that they vomited in a trash can in the bathroom when no one was around and is obviously well is certainly not an emergent issue. Often they vomit from coughing, or little kids choke and have a bad gag reflex, or they get stressed out. Vomiting is not always an emergency or even always an indicator of sickness.
5. Bee Sting: This is self explanatory. Bee stings hurt like crazy and should be handled right away, especially for a person who may be allergic to bees (documented allergy), or a person who is exhibiting symptoms of an allergic reaction (you might not always know they are allergic till it happens.)
6. Burning Up: Obvious fever, feels hot to touch. Fever over 100.4 should be sent home and stay home until 24 hours fever free (as a general guideline but some districts may have different rules).
7. Big Bump: Witnessed head injuries resulting in bruises, bumps, change in mental status or bleeding. “I bumped my head on a wall while in the bathroom/walking down the hall/etc etc” and they don’t have any concerning symptoms then it is safe to wait for the nurse to be available. Chances are, when they wait a few minutes they will forget about it.
8. Seizures: A student or an adult who is having a seizure should be addressed immediately. Call the nurse right away and note the exact time the seizure started so the nurse can time it. In general a seizure lasting greater than 5 minutes will require a call to 911 and possibly emergency medications if available.
9. Allergic Reactions: Someone who is short of breath, has hives, wheezing, facial swelling, tongue swelling, difficulty speaking, change in mental status, loss of consciousness, or has a known allergy and has been exposed to the known allergen should emergently see the nurse (or call the nurse to come to the scene). Hopefully the student has an Epi-pen if there is a known allergy but 911 and parents should likely be called depending on the situation.
10. Diabetic Emergencies/Management: A student who is a known diabetic and is experiencing loss of consciousness, changes in mental status (drowsy, confused, speech slurred) should be seen immediately. A student who is a known diabetic and feels that he needs a blood sugar check or feels unwell should be permitted to see the nurse immediately. A student who has scheduled times to manage blood sugars and insulin should see the nurse at the correct times.
11. Any student with a known medical condition that may require nursing intervention should be sent to the nurse as soon as possible.
What is NOT considered an emergency?
1. Potty Accidents: For my district potty accidents are not a nursing issue. The students should have extra clothes but if they don’t then parents should be called to bring them clean clothes. Check with your nurse to see what procedure is.
2. Seasonal Allergies: There is nothing the school nurse can do to manage seasonal allergies in school unless a student has medications that have been ordered by the doctor and the proper paperwork to dispense it. In general, if a student has allergies then it should be managed at home. A parent can always be called to address the issue if needed but it is not an emergent issue.
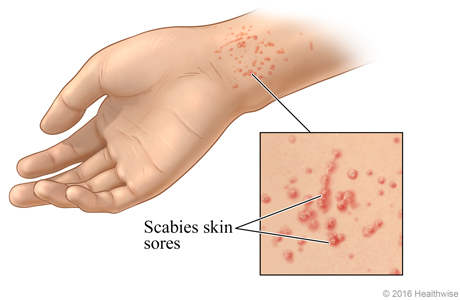
3. Mosquito bites/bug bites (aside from bee stings): In general, not an emergency. The nurse (in my district) can administer Hydrocortisone cream to an itchy bug bite but for the most part they have to wait it out.
4. Loose Teeth: Definitely not an emergency. A teacher is more than welcome to explain to a student that loose teeth are a natural, normal part of life and need no intervention aside from wiggling it till it comes out and the occasional mouth rinse if bleeding. Loose teeth may bleed, and they may be sore but such is life. Some nurses may be comfortable with pulling teeth but I choose not to do that as I feel it is a procedure that some parents may not prefer I do. It’s safer to just not do it.
5. Minor cuts and scrapes with or without bleeding: if the nurse is not available then the student can wait. If the teacher has bandaids then they may give one. A student may stay in class until it is an appropriate time to leave.
6. Dirty Clothes/got water on them/spilled food: This is not an emergency. Water dries, food can be wiped off. Chronically unkempt students should be addressed by the nurse and/or the counselor but it is not emergent to leave a class and manage unless the teacher feels it is an appropriate time.
Another idea that I learned that one could try is a “sick bench” for recess. In general students should not be leaving recess and lunch to visit the nurse as they have greater ability to wander or be away from their class without permission. Often, if they complain that they are sick at recess, have a tummy ache, or bumped themselves on something they can have a time out on the sick bench and take a break. You will notice that often waiting a few minutes cures them. Pain subsides, tummy aches from running around and playing hard will subside on their own.
A teacher or staff member has the ability to triage students health needs and make the call if they need to leave class right away and see the nurse or if they need to wait until the current lesson is finished before leaving. As always, everyone has the option to call the nurse and ask questions or discuss issues they have concerns about.
This is not an issue of “the nurse doesn’t want to see kids” but an issue of trying to keep the kids in their classes and cut out extraneous wandering about the school, and staying out of class. Our responsibility is keeping butts in seats as much as possible by keeping sick kids out and healthy kids in their classes.
Update: Here is a Google Slide deck of this article for your convenience: https://www.teacherspayteachers.com/Product/Is-It-An-Emergency-presentation-8154471