Click Here to access and follow my new website!
It’s more user friendly, search bar is available now, and my books are all in one place.
Comment and let me know what you would like to see from me on there! I’ll be adding more to it soon!
I’m talking about the real things you need to know as a school nurse.
By Simar Bajaj

The potentially fatal disease diphtheria is caused by bacteria — the club-shaped, Gram-positive, Corynebacterium diphtheriae bacilli shown in this microscope photo.
CDC via AP
It had been over 30 years since the last case of diphtheria was seen in Guinea. So when patients began showing up six months ago with what looked like flu symptoms — fever, cough and sore throat – doctors weren’t alarmed. Until the children started dying.
That’s when they realized that this longtime scourge, long quashed by vaccination, was back.
As of December 2023, there have been around 25,000 cases of diphtheria in West Africa and 800 deaths. In Guinea, the cases were clustered in Siguiri, a rural prefecture in the country’s northeast, and early data showed that 90% occurred in children under the age of 5.
Diphtheria is a highly contagious bacterial infection spread through direct contact with infected sores or ulcers but primarily through breathing in respiratory droplets. The bacteria then releases toxins, causing inflammation that blocks the airways; a thick mucus-like substance (called a “pseudomembrane”) can form at the back of the throat.
“This can kill by suffocating the patient,” says Adélard Shyaka, medical coordinator for Doctors Without Borders in Guinea. “But also the toxin moves through the body and can damage the heart, the kidneys, the nervous system.” Such damage — via suffocation, myocarditis, kidney failure and nerve malfunctioning — means diphtheria is fatal in up to 50% of cases without treatment.
The disease, which was a global scourge for much of the 20th century, is also almost entirely preventable through vaccination. After the diphtheria inoculation was included on the World Health Organization’s essential vaccine list in the 1970s, cases decreased dramatically worldwide. “Now, it’s an almost forgotten disease,” says Shyaka.
But that doesn’t mean this outbreak is surprising, according to Ankur Mutreja, a global health specialist with the Cambridge Institute of Therapeutic Immunology and Infectious Disease. “Diphtheria is and has always been a disease of poverty,” he emphasizes, with social unrest and poor vaccination coverage explaining most outbreaks nowadays. “It’s not just the West Africa outbreak but numerous other [recent] outbreaks — after the earthquake in Haiti, after war in Syria, in Bangladesh when the Rohingyas were displaced in 2017,” Mutreja says.
Guinea was particularly vulnerable because of its low diphtheria vaccination rate – only 47% in 2022, with the hardest-hit Siguiri prefecture having even lower coverage at 36%. COVID-19 disrupted routine vaccination campaigns in West Africa and was associated with an uptick in vaccine mistrust, Mutreja says. But for diphtheria and other preventable childhood illnesses, the immunization problem predated the pandemic due to supply chain difficulties, insufficient funding, and complacency, among other reasons, leaving the region vulnerable to a cluster of cases swelling into an outbreak.
In Guinea, Doctors Without Borders says its staff has supported local health workers in addressing diphtheria. Together, they’ve reduced mortality at Siguiri’s Center for the Treatment of Epidemics from 38% to 5% over the past few months. Patients with mild symptoms are sent home with antibiotics, while more severe cases are admitted to the hospital and treated with an antitoxin, as appropriate.
However, shortages of both vaccines and antitoxins continue to hamper a full-scale response to the diphtheria outbreak, according to Louise Ivers, an infectious disease physician and the director of the Harvard Global Health Institute. Presently, only two or three companies make the antitoxin, and each batch of 1,500 doses takes about four weeks to prepare, harvested from horse blood. “Nobody wants to make it,” says Ivers, because of how rarely this antitoxin is usually needed – there were fewer than 9,000 cases globally in 2021 – and how impoverished communities facing diphtheria tend to be. “That puts it into the category of low likelihood of commercial profit.”
The only sure way this outbreak ends is through vaccination, suggests Ivers, who has firsthand experience responding to diphtheria in Haiti between 2003 and 2012. However, similar market dynamics may help explain the global shortage of diphtheria vaccines. “If we can catch back up with DPT [vaccines] and diphtheria boosters and get our communities highly vaccinated,” she says, “then we can prevent outbreaks.”
But the scarcity of vaccines means they’ve only been available for patients and their close contacts in Siguiri. As diphtheria continues to spread in Guinea, Mutreja worries about growing antibiotic resistance and the spread of new variants, which could render existing antitoxins and vaccines ineffective. In fact, resistance has already been increasing, decade over decade, for the past 122 years, as Mutreja described in a 2021 study in Nature Communications. “We mustn’t take our eye off the ball with diphtheria. Otherwise, we risk it becoming a major global threat again, potentially in a modified, better-adapted form,” he says.
While this present surge of diphtheria cases is indeed unprecedented for West Africa, it is really a symptom of larger issues in global health, including insufficient infectious disease surveillance, poor vaccination rates and scarcity of public health resources, suggests Shyaka. He’s not only worried about Guinea’s current diphtheria outbreak but also what other diseases are on the horizon, including meningitis, measles and whooping cough.
“The resurgence of diphtheria is an important indicator that we are far in the red zone of outbreaks — of vaccine-preventable outbreaks.”
Simar Bajaj is an American journalist who has previously written for The Atlantic, TIME, The Guardian, Washington Post and more. He is the recipient of the Foreign Press Association award for Science Story of the Year and the National Academies award for Excellence in Science Communications.
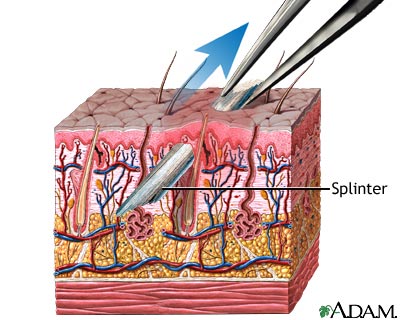
Getting splinters out can be a tough job sometimes. Not all school nurses prefer to remove splinters but in case you do here are some tips and tricks to hopefully make it a little easier.
First and foremost, if you do not prefer to remove splinters as some do, it is perfectly reasonable to clean the area, cover with a bandaid and let the parent know so they can handle it at home. Many nurses feel that it is outside of their scope of practice to “dig” for a splinter that is not easily removed as it is a more invasive procedure that could be considered “surgery”. If the splinter is sticking out or easily removed then it is ok to grab it with tweezers and remove it or soak it and give it a try but if it is too deep and requires a lot of digging then stop and inform the parent.
If you want to try and get it out here are some tips to make it easier. Before attempting to remove anything make sure that you clean the area well and use clean/sterile packaged equipment, make sure the student does not have an allergy to items used. Always stop if they can’t tolerate the removal attempt.

When all else fails and you can’t get it out without causing excessive pain or bleeding, clean it, cover it and notify parent. They can take the child to the doctor for removal.

https://www.nursingcenter.com/static?pageid=1037067
https://www.quickanddirtytips.com/articles/8-tricks-for-removing-splinters
https://www.aad.org/public/everyday-care/injured-skin/burns/remove-splinters
https://www.cincinnatichildrens.org/health/s/splinters
https://kidshealth.org/en/parents/splinters-sheet.html?ref=search

Mentha x piperita
Peppermint (Mentha piperita), a popular flavoring for gum, toothpaste, and tea, is also used to soothe an upset stomach or to aid digestion. It has a calming and numbing effect, and is often used to treat headaches, skin irritation, nausea, diarrhea, menstrual cramps, flatulence, and anxiety associated with depression. It is also an ingredient in chest rubs used to treat symptoms of the common cold. In test tubes, peppermint kills some types of bacteria, fungi, and viruses, suggesting it may have antibacterial, antifungal, and antiviral properties. Menthol and methyl salicylate, the main ingredients in peppermint, have antispasmodic effects, with calming effects on the gastrointestinal tract. Several studies support the use of peppermint for indigestion and irritable bowel syndrome.
Peppermint calms the muscles of the stomach and improves the flow of bile, which the body uses to digest fats. As a result, food passes through the stomach more quickly. However, if your symptoms of indigestion are related to a condition called gastroesophageal reflux disease or GERD, you should not use peppermint (see “Precautions” section).
Peppermint relaxes the muscles that allow painful digestive gas to pass.
Several studies have shown that enteric-coated peppermint capsules can help treat symptoms of IBS, including pain, bloating, gas, and diarrhea. (Enteric-coated capsules keep peppermint oil from being released in the stomach, which can cause heartburn and indigestion.) However, a few studies have shown no effect. One study examined 57 people with IBS who received either enteric-coated peppermint capsules or placebo twice a day for 4 weeks. Of the people who took peppermint, 75% had a significant reduction of IBS symptoms. Another study comparing enteric-coated peppermint oil capsules to placebo in children with IBS found that after 2 weeks, 75% of those treated had reduced symptoms. Finally, a more recent study conducted in Taiwan found that patients who took an enteric-coated peppermint oil formulation 3 to 4 times daily for 1 month had less abdominal distention, stool frequency, and flatulence than those who took a placebo. Nearly 80% of the patients who took peppermint also had alleviation of abdominal pain.
Peppermint, when applied topically, has a soothing and cooling effect on skin irritation caused by hives, poison ivy, or poison oak.
One small study suggested that peppermint applied to the forehead and temples helped reduce headache symptoms.
Peppermint and its main active agent, menthol, are effective decongestants. Because menthol thins mucus, it is also a good expectorant, meaning it helps loosen phlegm and breaks up coughs. It is soothing and calming for sore throats (pharyngitis) and dry coughs.
Peppermint plants grow to about 2 to 3 feet tall. They bloom from July through August, sprouting tiny purple flowers in whorls and terminal spikes. Dark green, fragrant leaves grow opposite white flowers. Peppermint is native to Europe and Asia, is naturalized to North America, and grows wild in moist, temperate areas. Some varieties are indigenous to South Africa, South America, and Australia.
The leaves and stems, which contain menthol (a volatile oil), are used medicinally, as a flavoring in food, and in cosmetics (for fragrance).
Peppermint tea is prepared from dried leaves of the plant and is widely available commercially.
Peppermint spirit (tincture) contains 10% peppermint oil and 1% peppermint leaf extract in an alcohol solution. A tincture can be prepared by adding 1 part peppermint oil to 9 parts pure grain alcohol.
Enteric-coated capsules are specially coated to allow the capsule to pass through the stomach and into the intestine (0.2 mL of peppermint oil per capsule).
Creams or ointments (should contain 1% to 16% menthol)
DO NOT give peppermint to an infant or small child. Peppermint oil applied to the face of infants can cause life-threatening breathing problems. In addition, peppermint tea may cause a burning sensation in the mouth. For digestion and upset stomach in older children: 1 to 2 mL peppermint glycerite that is specially formulated for children, per day.
The use of herbs is a time-honored approach to strengthening the body and treating disease. Herbs, however, can trigger side effects and interact with other herbs, supplements, or medications. For these reasons, you should take herbs with care, under the supervision of a health care provider.
DO NOT take peppermint or drink peppermint tea if you have gastroesophageal reflux disease (GERD — a condition where stomach acids back up into the esophagus), or hiatal hernia. Peppermint can relax the sphincter between the stomach and esophagus, allowing stomach acids to flow back into the esophagus. (The sphincter is the muscle that separates the esophagus from the stomach.) By relaxing the sphincter, peppermint may actually worsen the symptoms of heartburn and indigestion.
The amount of peppermint normally found in food is likely to be safe during pregnancy, but not enough is known about the effects of larger supplemental amounts. Some experts even recommend modest amounts of peppermint tea to help alleviate nausea during pregnancy. Speak with your provider before using peppermint or any other herbal products during pregnancy.
Never apply peppermint oil to the face of an infant or small child, as it may cause spasms that inhibit breathing.
Peppermint may make gallstones worse.
Large doses of peppermint oil can be toxic. Pure menthol is poisonous and should never be taken internally. It is important not to confuse oil and tincture preparations.
Menthol or peppermint oil applied to the skin can cause a rash.
Non enteric-coated capsules and peppermint oil can lead to heartburn.
This drug, which is usually taken to prevent rejection of a transplanted organ, suppresses the immune system. Peppermint oil may slow down the rate at which the body breaks down cyclosporine, meaning more of it stays in your bloodstream. DO NOT take peppermint oil if you take cyclosporine.
If you take peppermint capsules at the same time as drugs that lower the amount of stomach acid, the enteric-coated peppermint capsules may dissolve in the stomach instead of the intestines. This could reduce the effects of peppermint. Take peppermint at least 2 hours before or after an acid-reducing drug. Antacids include:
Test tube studies suggest peppermint may lower blood sugar, raising the risk of hypoglycemia (low blood sugar).
Since peppermint works on the liver, it may affect medications that are metabolized by the liver (of which there are many). Speak with your health care provider.
Some animal studies suggest that peppermint may lower blood pressure. If you take medications to lower blood pressure, taking peppermint also might make their effect stronger.
Agarwal V, Lal P, Pruthi V. Effect of plant oils on Candida albicans. J Microbiol Immunol Infect. 2010;43:447-451.
Alam MS, Roy PK, Miah AR, et al. Efficacy of Peppermint oil in diarrhea predominant IBS – a double blind randomized placebo – controlled study. Mymensingh Med J. 2013; 22:27-30.
Blumenthal M, Goldberg A, Brinckmann J. Herbal Medicine: Expanded Commission E Monographs. Newton, MA: Integrative Medicine Communications; 2000:297-303.
Cappello G, Spezzaferro M, Grossi L, Manzoli L, Marzio L. Peppermint oil (Mintoil) in the treatment of irritable bowel syndrome: a prospective double blind placebo-controlled randomized trial. Dig Liver Dis. 2007;39:530-536.
Cash BD, Epstein MS, Shah SM. A novel delivery system of peppermint oil is an effective therapy for irritable bowel syndrome symptoms. Dig Dis Sci. 2016;61(2):560-571.
Ford AC, Talley NJ, Spiegel BM, et al. Effect of fibre, antispasmodics, and peppermint oil in the treatment of irritable bowel syndrome: systematic review and meta-analysis. BMJ. 2008;337:a2313.
Herro E, Jacob SE. Mentha Piperita (peppermint). Dermatitis. 2010;21:327-329.
Imagawa A, Hata H, Nakatsu M, et al. Peppermint oil solution is useful as an antispasmodic drug for esophagogastroduodenoscopy, especially for elderly patients. Dig Dis Sci. 2012;57:2379-2384.
Inamori M, Akiyama T, Akimoto K, et al. Early effects of peppermint oil on gastric emptying: a crossover study using a continuous real-time 13C breath test (BreathID system). J Gastroenterol. 2007;42:539-542.
Kline RM, Kline JJ, Di Palma J, Barbero GJ. Enteric-coated, pH-dependent peppermint oil capsules for the treatment of irritable bowel syndrome in children. J Pediatr. 2001;138:125-128.
Korterink JJ, Rutten JM, Venmans L, Benninga MA, Tabbers MM. Pharacolgic treatment in pediatric functional abdominal pain disorders: a systematic review. J Pediatr. 2015;166(2):424-431.e6.
Lane B, Cannella K, Bowen C, et al. Examination of the effectiveness of peppermint aromatherapy on nausea in women post C-section. J Holist Nurs. 2012;30:90-104.
Madisch A, Holtmann G, Mayr G, Vinson B, Hotz J. Treatment of functional dyspepsia with a herbal preparation. A double-blind, randomized, placebo-controlled, multicenter trial. Digestion. 2004;69:45-52.
Magge S, Lembo A. Complementary and alternative medicine for the irritable bowel syndrome. Gastroenterol Clin North Am. 2011;40(1):245-253.
McKay DL, Blumberg JB. A review of the bioactivity and potential health benefits of peppermint tea (Mentha piperita L). Phytother Res. 2006;20:619-633. Review.
Rakel D. Integrative Medicine. 3rd ed. Philadelphia, PA. Elsevier Saunders; 2012.
Shen YH, Nahas R. Complementary and alternative medicine for treatment of irritable bowel syndrome. Can Fam Physician. 2009;55:143-148.
Yamamoto N, Nakai Y, Sasahira N, et al. Efficacy of peppermint oil as an antispasmodic during endoscopic retrograde cholangiopancreatography. J Gastroenterol Hepatol. 2006;21:1394-1398.

For immediate release: January 05, 2024
Published by: Board of Health, Department of Public Health
Contact: Health Department phlpublichealth@phila.gov
PHILADELPHIA—The City continues to respond to the ongoing measles outbreak in Philadelphia.
Current situation
Today, the Health Department reports a total of 5 confirmed and 3 presumed cases of measles associated with this outbreak. Currently, 3 of these cases are hospitalized with measles.
The Health Department is posting regular updates on the City’s website. Check for the latest.
Today’s updates
The Health Department announced that all City Health Centers have the MMR vaccine which can protect you from measles. Any child in Philadelphia can receive free vaccines at City Health Centers. Call Center Operators can be reached at 215-685-2933 to set up an appointment.
Philadelphia has high vaccination rates, with at least 93% of children fully vaccinated against measles by age 6. If you or your child has not yet been vaccinated, call today to get vaccinated.
“If you have not yet been vaccinated against measles or have not vaccinated your children or are 12 months or age or older, reach out to your healthcare provider to do so immediately,” said Health Commissioner Dr. Cheryl Bettigole.
For a limited time, Health Center 3 (555 S 43rd St.), Health Center 4 (4400 Haverford Ave.), and Health Center 5 (1900 N 20th St.) are also offering walk-in MMR vaccinations to any Philadelphia resident, Monday through Thursday 10am -12noon and 1p-3p.
All of these vaccines are free at the City Health Centers. There is no need for an ID, just a piece of mail with your address on it will confirm your residency.
The Health Department reminds Philadelphians that vaccination is the very best way to protect yourself and your children against measles and many other diseases.
The Health Department also released the following timeline to help detail the history of this quickly evolving situation.
Press notes
The Health Department is coordinating media interviews with Health Commissioner Dr. Cheryl Bettigole. Press are instructed to submit all interview and information requests on the measles outbreak to phlpublichealth@phila.gov.
Press is not being offered access to any of the Health Centers vaccinating clinics at this time in order to preserve anonymity of patients. This may change as the response continues.
For more basic information on measles and vaccines, please see the Health Department’s blog post.
See full press release here: https://www.phila.gov/2024-01-05-health-department-update-on-measles-outbreak-january-5-2024/

Image from https://www.2foodtrippers.com/best-american-candy/
Neha Prathivadi
The expression “sugar rush” is one that has been in our vocabularies since our early childhood days. Many parents are concerned about their children’s consumption of candy and other sugary foods, because they fear it will lead to overexcitement and hyperactivity. However, is there actually a link between sugar and hyperactivity in children? Researchers seem to disagree.
The concept of the “sugar rush” originated from the theory that since sugar is a source of energy for our bodies, consuming more sugar should lead to higher energy levels. In reality, our bodies don’t break down all the sugar immediately. Rather, we store it and use small amounts when needed, so we shouldn’t actually show signs of hyperactivity after eating large amounts of sugar.
An analysis of multiple research studies found that sugar does not impact the behavior or mental performance of children. So, if there is no impact, how do we explain children appearing “hyper” after consuming sugar? The answer may be confirmation bias. Most kids tend to eat sugary foods in fun settings, like birthday parties or family holidays. Our minds may falsely link the excitement surrounding the event to the sugar.
Another interesting fact is that sugar blocks the hypothalamic pituitary adrenal (HPA) axis, which is a component of our brain that is associated with stress. Therefore, sugar might lessen stress levels and could actually calm us.
So far, there is no evidence to show a connection between sugar and hyperactivity in children. Nevertheless, it is still important to be aware of what you are consuming in order to maintain a healthy diet and lifestyle. So have fun and enjoy your occasional ice cream, cookie, or candy, but make sure to snack in moderation!
Links:
Fevers are often a misunderstood symptom of illness. Why do we get them and what do we do about them?
A fever is a temporary rise in body temperature. It’s one part of an overall response from the body’s immune system. There are multiple reasons for fevers including infections, viruses, heat exhaustion, sometimes immunizations, and sometimes certain diseases like cancers or inflammatory illness can cause a fever.
When an invader enters the body the immune system begins a cycle of macrophages, white blood cells, monocytes, and lymphocytes to begin a cytokine induction which fights the invader. This is outwardly exhibited by an appreciable rise in body temperature – usually about 100.4 (give or take a tenth of a degree) and above is considered a fever.
Myth: If your perceived “normal” body temperature is always 97.6 and you have a temperature of 99.6 it’s considered a fever. Not entirely true! Yes it is a slight elevation in temperature and can indicate illness but it is not concerning. A temperature of 99.6 – 100.3 can be considered a low grade fever depending on the other symptoms and age of the patient. Body temperature can rise and lower for various reasons such as hot weather, exercising, hormones (if you’re trying to conceive and tracking ovulation, you would find out that when ovulation occurs the basal body temperature increases slightly but that’s for another post), or teething in infants. Don’t worry if a person’s temperature is in the 99’s but they have no other real symptoms.

Per Penn Medicine: Contact a provider right away if your child:
Contact your provider right away if you are an adult and you:
Call 911 or the local emergency number if you or your child has a fever and:


What illnesses can cause a fever? The list is very long and we aren’t diagnosing but in a school setting we might consider:
Do you have any hot tips, fast facts or info about managing fevers that we need to know about? Please comment, email, or join my facebook group and let me know what you think!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7122269/
https://www.prevention.com/health/a20429676/10-fever-remedies/
January is National Eye Care Month. I recently learned about a condition called Convergence insufficiency that affects the eye muscles but rarely the actual vision of the patient. It is often missed or misdiagnosed as good vision but dyslexia or behavioral problems. Please check out this article from the American Optometric Association.
Convergence insufficiency (CI) is a common, yet not frequently diagnosed eye coordination problem in which the eyes drift outward when reading or doing close work.
Convergence insufficiency (CI) is caused by a simple “lack of proper communication” between the nerves and the muscles that control eye movements. The muscles surrounding the eye (there are six) are plenty strong, but the nerves that control these muscles are not sending the proper message to turn inward enough to aim at the target (page or screen).
There are many symptoms listed below. An easy way to explain how it really feels is by comparing your eyes when reading to driving along the interstate. When driving is normal, your car is usually in one lane but there are two lanes that can be used, thus giving a feeling of comfort. When you enter a construction zone, squeezed down to one lane with concrete barriers on each side of you, there is still plenty of room for your car, but not as much as with two lanes. The result is you most likely will slow down, hold the wheel tighter, stiffen your shoulders, and overall feel more stressed.
Your eyes have a similar comfort zone called the fusional range. Your fusional range is how far inward and how far outward your eyes can move and still see single and comfortable. If that range is narrow, just like the construction zone, you will slow down and feel more stressed when you are reading because there is one thing your brain hates and that is seeing double. In order to not see double, eyes start working very hard to maintain single vision.
This can lead to a multitude of symptoms including eyestrain (especially with or after reading), plus:
CI can almost be diagnosed by listening to the patient describe their symptoms. If these symptoms (all or some) are noted, extra testing can be performed to diagnose or rule out CI. It is important to note that most routine eye exams will not include specific testing for CI, so it is important that the patient or parent explains in detail the symptoms he/she is having. That will signal the doctor to add extra testing to see how well the eyes work together.
Treatment can be active or passive. Active treatment involves fairly intense eye exercises that retrain the nerves to aim the eyes properly and increase the fusional range. The most successful treatment involves home plus office therapy. The least successful involves an older form of treatment called “pencil push-ups”. Pencil push-ups can help but only when incorporated into a complete therapy program. Active treatment can last up to 90 days or more and typically the results are permanent. Passive treatment is more like a crutch that works only when in place. Prisms can be incorporated into reading glasses that redirect light entering the eyes. Think of it as the lenses doing the work the nerves don’t know how to do.
In the case of CI, treatment is part of the prevention. This is because if the condition is not properly treated, it can progress into a much more serious condition called intermittent exotropia. This is the brain’s answer to coping with double vision and the stress of eyes not working as a team. The eyes may drift further apart and simply begin working independently rather than as a team. This can lead to a whole host of new problems. Our brain is wired for two eyes to work together and when this doesn’t happen, the problems begin to go beyond discomfort while reading. The use of one eye is suppressed.
Suppression of vision in one eye causes loss of binocular (two-eyed) vision and depth perception. Poor binocular vision can have a negative impact on many areas of life, such as coordination, sports, the judgment of distances, eye contact, motion sickness, etc. Consequently, a person with convergence insufficiency who is suppressing one eye can show some or all of the following symptoms:
In summary, CI is a common but frequently missed diagnosis (one can have uncorrected vision in each eye of 20/20 vision and still have CI so screenings at work and school will totally miss it). CI is also very treatable if diagnosed. However, treatment is patient intensive. If the patient doesn’t do the therapy, there will be no improvement.