Update: I was searching online today to find out if Trix cereal is tree nut free (it is!) and found this website and ap that helps you find out if food has certain allergy ingredients! It’s so amazing! It’s called Spoonful. All you have to do is type in the name of the product and it will tell you if there are specific allergens in that food. You can also download the free ap and use it to scan the barcode on foods to get the info for everything from gluten, low FODMAP, nuts, eggs, dairy, etc!
Your child has an allergy to something and you have to send them off to school. That can be scary for many parents but we’ve got your back here at school! Here is some information your school nurse wants you to know about having allergies at school.
What is an anaphylactic allergy or anaphylaxis? Anaphylaxis or allergy to foods/medicines is a different issue than intolerance to foods or substances. When a person has anaphylaxis to a substance it means they have a true allergy which can cause their airways to swell and tighten making breathing difficult, blood pressure can drop causing them to pass out, they get itchy red hives all over or in different places, they may be coughing or vomiting.
Anaphylaxis is a life threatening emergency that requires epinephrine as soon as possible to reverse the allergic reaction. Usually the allergic reactions tend to be worse with each exposure so the first or second exposure may be mild but continuing exposures can become worse each time.
An intolerance to a substance is generally unwanted side effects from a drug or food such as lactose intolerance versus cows milk allergy. Lactose intolerance means the persons body does not process the component of cow’s milk and can give them nausea, diarrhea, or upset stomach but rarely worse symptoms than that. A true allergy generally consists of the above mentioned symptoms. A person may be intolerant to a medication such as Amoxicillin where they have diarrhea or upset stomach or they may have a true allergy that involves hives and anaphylaxis. It’s important to know the distinction as each would be treated differently and intolerance is less emergent than anaphylaxis.
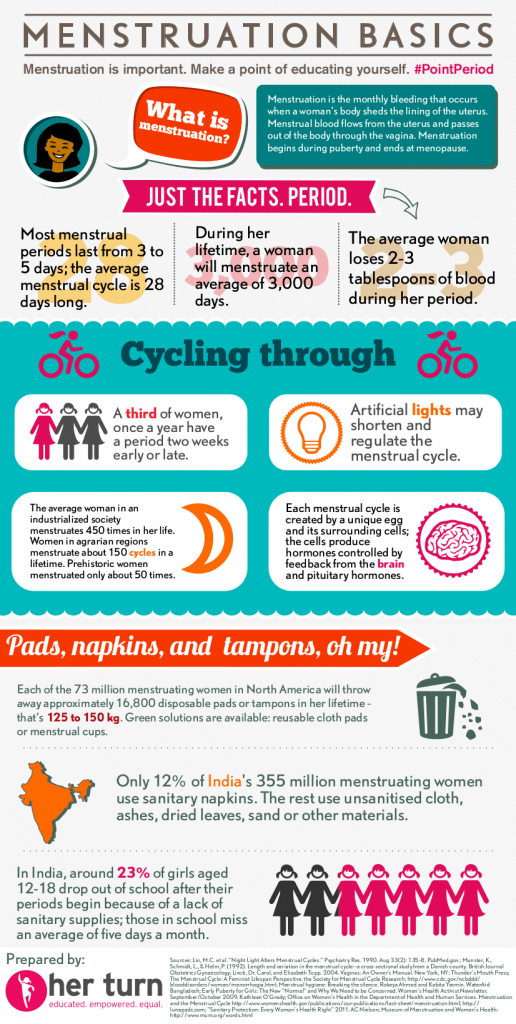
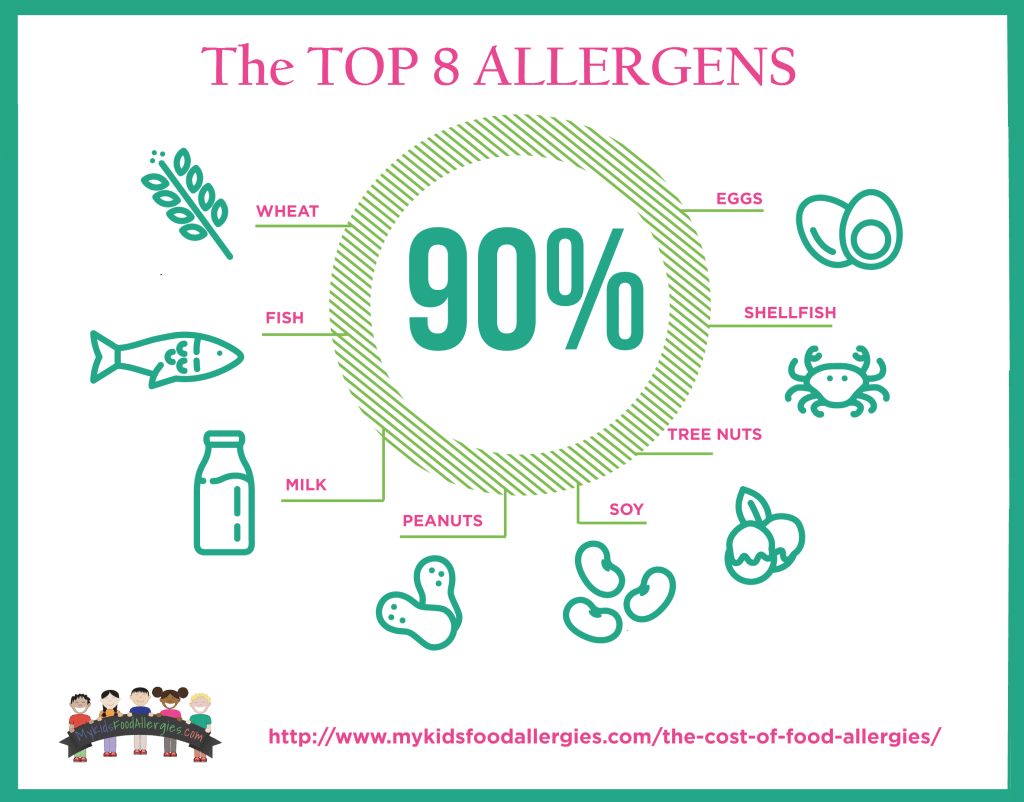
Common triggers for anaphylaxis can include foods like peanuts, various nuts, cows milk, eggs, some antibiotics and other medications, seafood, shellfish, strawberries, and various fruits and vegetables. There is no end to the substances that someone could be allergic to but these are some of the most common ones. One has to be careful to read labels and ask questions to be aware of the ingredients of certain foods as they may have an allergen in them that you were unaware of. One should also be aware if their food is cooked at or prepared in a facility or kitchen that is also using the allergen they are allergic to as the cross contamination could cause a reaction.
What do we do when someone has an anaphylactic allergy? In school, once the emergency is recognized, the Epi-pen will be administered as soon as possible – in my school the Epi-pens are housed in the nurses office and they would call me or radio me to get to the scene with it asap, older students would be allowed to self carry. In some schools the Epi-pen is with the student at all times and the student or the closest adult trained staff member will administer it. The second step is to call 911 because even if the reaction is reversed it can begin again so EMS is needed. If the doctor has ordered Benadryl we will also give that right away if the student is awake and able to take it. Someone will be calling the parent or guardian of the student immediately. The treatment, 911, and parent phone call can all be done at the same time by different staff members.

So what can you do when you send your child to school when they have an anaphylactic allergy to a food or substance?
- Communicate. You should let your child’s teacher know, let the school nurse know, let the administrators know, and you can even let the food service people know as well to avoid any accidental exposure at meal times. As the school nurse, I do provide the relevant people information about specific student’s allergies so everyone is on the same page and knows to be careful. This can be done with a phone call, email, or most importantly, a health form from a well check.
- Send an Epi-pen to school with your child and include the appropriate doctor’s orders as soon as possible. Check if your child’s doctor wants you to also provide Benadryl to accompany the Epi-pen (some do some don’t).
- Check if your child’s school has standing orders and stock Epi-pens – mine does not and the parents must provide it always but many schools have standing orders and stock Epi-pens.
- Always be sure to provide the school with correct and updated emergency contact information. If your child does have an allergic reaction we will need to get ahold of you right away. Your contact information and allergy information should be with the student in case of emergency so we can call you as soon as possible.
- Consider placing a medic-alert bracelet on your child so everyone is reminded to avoid exposure.
- Make sure your child knows what an allergic reaction looks/feels like so they know what to do in case of exposure. They need to know to tell someone immediately if they are able to (some reactions are too fast for them to say anything and some kids just don’t know that anything is wrong until they are in full blown anaphylaxis).
- Make sure that your child knows how and when to use their Epi-pen. Most of the time the nurse or adult staff member would be administering the Epi-pen as soon as possible but there may be occasions when the student has the pen with them and is able to react faster. They should know what to do. You can even make sure your child’s siblings and friends know how to recognize symptoms and how to use the Epi-pen (if they are old enough) just to be safe.
- Find out what the policies are at your child’s school for managing food allergies. Is the whole school peanut-free? Just their class? Just their special lunch table? Not allergen free at all? You can ask for accommodations for your child if the school policies don’t align with your child’s needs – most likely the teachers, admins and health team will be able to come up with a plan that works for your child.
For school nurses:
What can the school nurse do to help manage and/or prevent anaphylaxis in their school?
Organize your Epi-pens and have them clearly labeled and available so you can grab it quickly and run if needed. Over the door shoe organizers work well for this, or if you have the means they sell really nice medication storage units. I also found this simple cubby unit that would be perfect for storing meds at your fingertips.
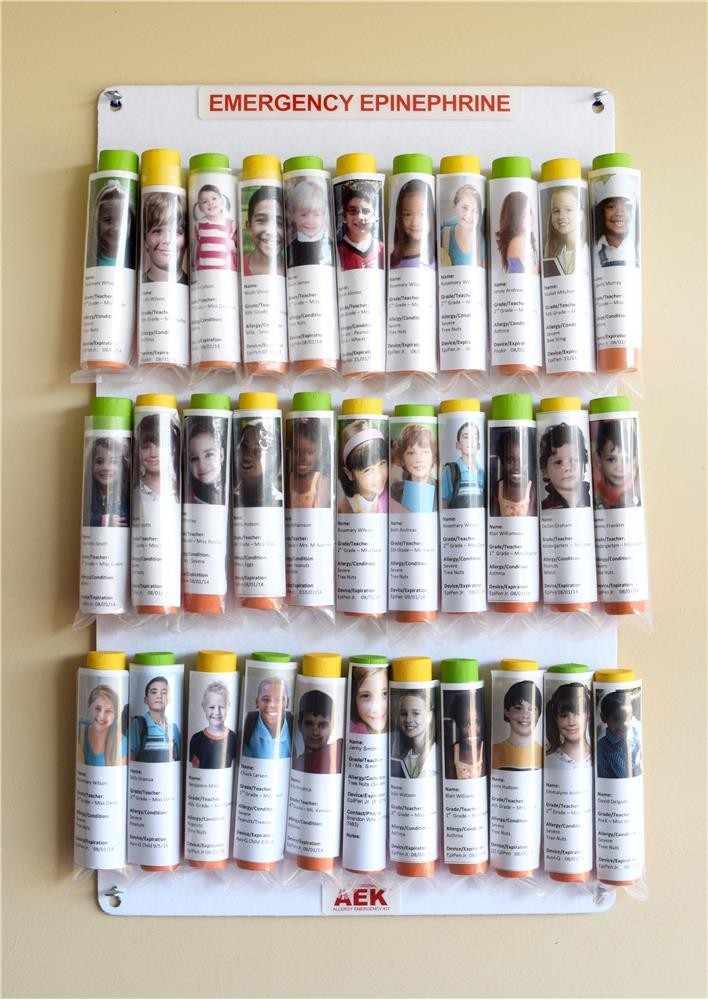
Keep all the parents information with the Epi-pens. Place a copy of their contact information, insurance information, health information, action plan, and anything else you might need to look up quickly with the Epi-pen so you can grab it all at once and not have to search for it.
Make sure your staff knows how to operate an Epi-pen, how to recognize anaphylaxis, and what steps they need to know to help manage an emergency. Education is crucial to recognizing and managing an allergic reaction quickly for optimal outcomes. Check out this presentation I made to educate my staff on how to use Epi-pens: Epi-pen
Educate staff on the procedure for handling an allergic reaction. They should know who to call, when to call, where the medications are and how to access them. There should be pre-established roles for who is calling 911, who is calling the nurse, who is calling the parent, and who is tending to the student. If this information is established prior to an emergency the management will hopefully flow better and have a better outcome. Think like a code situation – who’s wearing the red hat?
Make sure you provide the pertinent information about specific allergies to the students teachers, lunch people, and staff that needs to know. They don’t know what they don’t know so if they aren’t looking for it they might miss the beginning of a reaction or miss a possible exposure.
Establish a policy for your school for how exposure prevention to allergies will be handled. Decide if your facility will be completely allergen free – this works if you have multiple known allergies to one specific food (like peanut-free). You can have the students with allergies sit at a “safe table” in the lunch room but consider the fact that this has the potential to make the students feel singled out and possibly embarrassed (in my opinion embarrassment should be second to preserving life – if that is the best option for the students in your school then so be it). This is something to discuss with your administrators to decide how to proceed. In my school we do not separate anyone nor do we limit any specific foods due to allergies. We stay aware of the allergies and students are educated not to share food. Because my school is in a lower socioeconomic area, many students don’t have the choice to choose what foods they can bring and limiting their choices can lead to increased hunger in the students who don’t have allergies. The majority of my students receive the school lunches and breakfasts so the foodservice people are aware of who can’t have certain foods and avoid that. Also, the school meals are generally allergen free to reduce unintended exposures.

Sources: https://www.mayoclinic.org/diseases-conditions/anaphylaxis/symptoms-causes/syc-20351468
https://www.aaaai.org/conditions-and-treatments/allergies/anaphylaxis